Exposing the gender health gap
COVID-19 vaccine studies show women's health still sidelined

How does the vaccine impact menstrual cycles?
It is more than two years since the first case of the Coronavirus pandemic was reported in Wuhan, China.
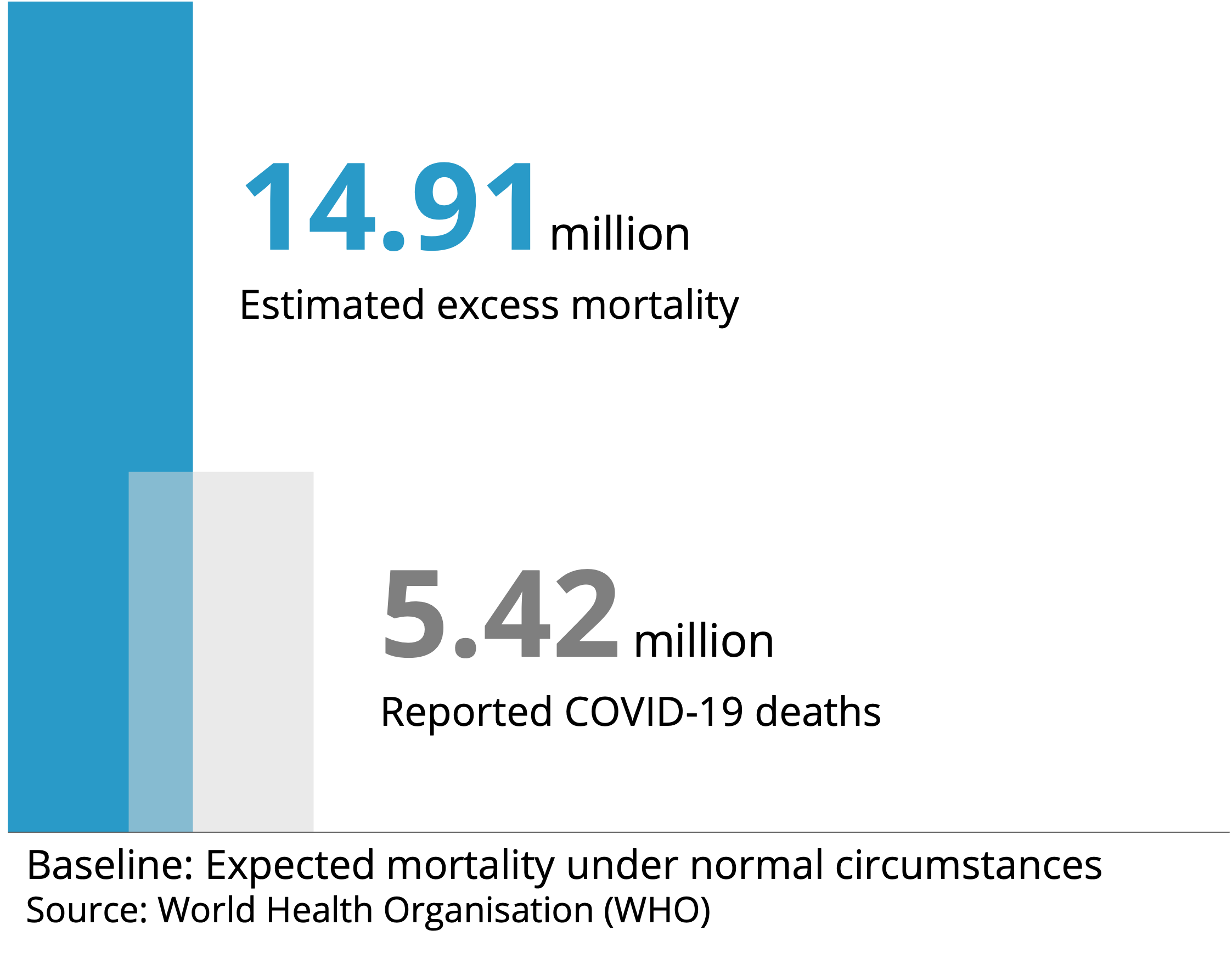
It caused mass disruption to people’s lives and significant loss of life, estimated by the World Health Organisation (WHO) at approximately 14.9million deaths between 1 January 2020 and 31 December 2021, as a direct or indirect result of COVID-19.
The race to develop and administer vaccinations was widely reported and on 8 December 2021, the NHS delivered the first clinically approved UK vaccination to 90-year-old Margaret Keenan, a record considering vaccine development often takes 10 to 15 years. Great care was taken to ensure the safety of the vaccine was not compromised by the speed of its delivery and WHO estimated in November 2021 that approximately 470,000 lives had been saved across 33 European countries as a direct result of the vaccine.
However, the pace of research in response to reports from individuals experiencing menstrual irregularity following the vaccine, was comparatively slow.
As of 29 March 2022, over 39,000 reports of menstrual changes or unexpected vaginal bleeding following COVID-19 vaccination had been made to the ‘Yellow Card’ surveillance scheme run by the UK Medicine and Healthcare Products Regulatory Agency (MHRA). Similar patterns were noticed in other countries and studies began.
The Norwegian Institute of Public Health found that among a cohort of 5,688 participants, 37.8% reported at least one change from normal, even in pre-vaccination cycles. The most common change reported was heavier than normal bleeding. A US study found the first dose of vaccine had no effect on timing of the subsequent period, while the second dose saw a delay of 0.45 days on average.
The 358 people in the study who received both doses of the vaccine in the same cycle experienced a 2.32 day delay to their next bleed and 10.6% of those experienced a change in cycle length of more than 8 days, deemed to be ‘clinically significant’.
In the UK, the 8 week interval between vaccine doses, compared to the 3 to 4 weeks typical in the US and Norway means it is impossible to receive both doses in the same cycle. However, results still suggest the vaccine impact cycles.
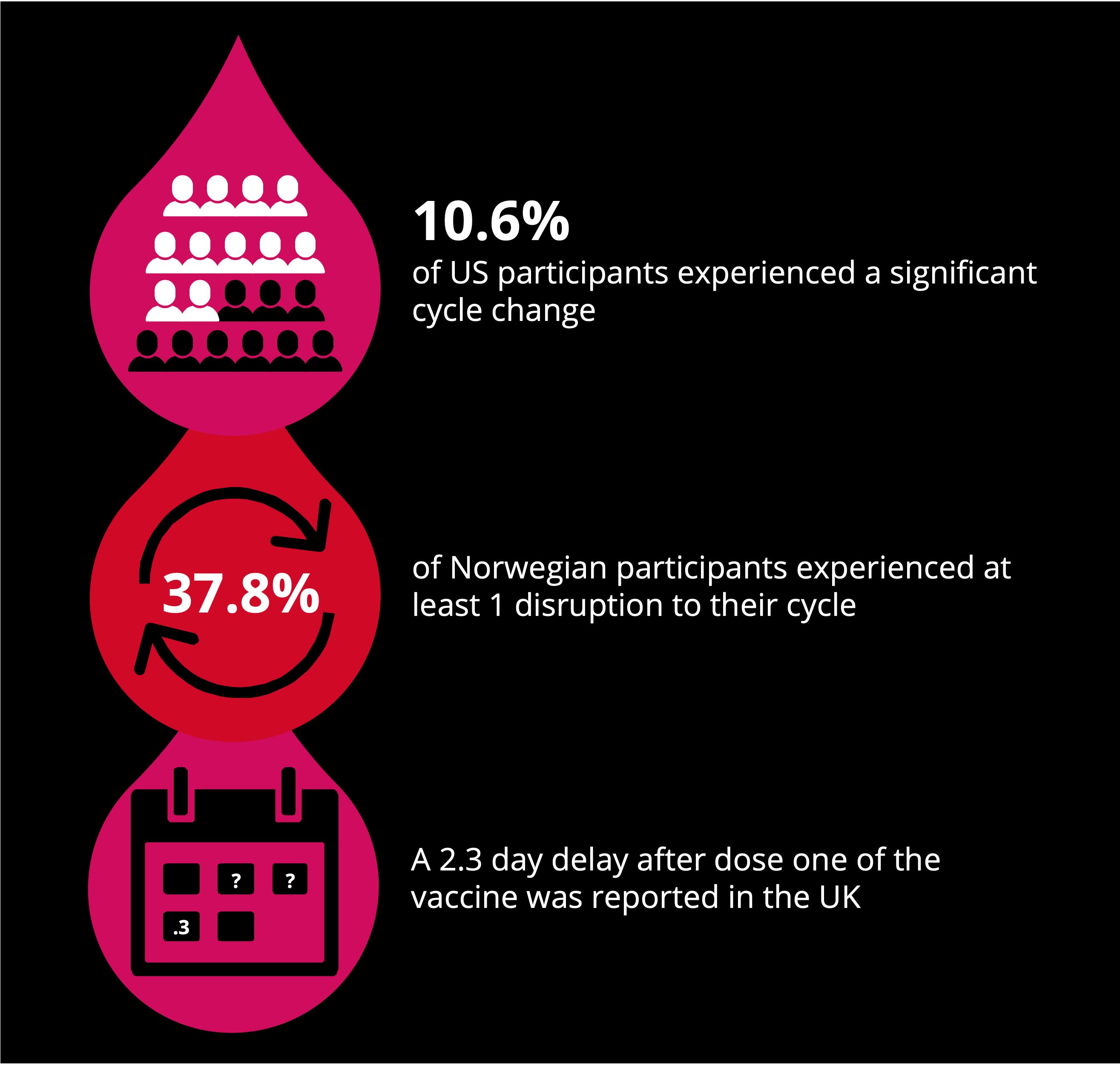
Dr Victoria Male led a team at Imperial in a study of 79 individuals who were asked to record at least three consecutive cycles during which they received at least one dose of the vaccine. The study found that either dose of the COVID-19 vaccine is associated with a delay to the subsequent period, a 2.3 day delay after dose one on average across the study, and 1.3 days after dose two.
In an article published in the British Medical Journal (BMJ), Dr Male described the results of the international studies as reassuring.
She said: “Changes to the menstrual cycle do occur following vaccination, but they are small compared with natural variation and quickly reverse.”
She added, however: “The fact that it has taken us so long to get here reflects the low priority with which menstrual and reproductive health is often treated in medical research.
“The widespread interest in this topic highlights how pressing a concern this is for the public. It’s time we started listening to them.”

Photo by Daniel Schludi on Unsplash
Nothing about us without us
In May of this year The Medicines and Healthcare products Regulatory Agency (MHRA) said they were still reviewing reports of suspected menstrual side effects from the Coronavirus vaccine.
They added: “The rigorous evaluation completed to date does not support a link between changes to menstrual periods and related symptoms and COVID-19 vaccines.
“While uncomfortable or distressing, period problems are extremely common and stressful life events can disrupt menstrual periods.”
Despite the MHRA’s interpretation of the studies, the voices of individual show that in some cases, changes to menstrual cycles after the vaccine were significant and had a big impact on people’s daily lives.
Below, two women speak about their experiences after receiving the Coronavirus vaccine:
*Zainab 26 received her first dose of the AstraZeneca (AZ) vaccine in March 2021 and a second dose of AZ in May of the same year. She has no other diagnosed conditions.
*Alice, 23, who received her first AZ dose in February 2021, and a second dose of Pfizer in May of the same year has been diagnosed with Premenstrual dysphoric disorder (PMDD), a very severe form of premenstrual syndrome, which causes a range of emotional and physical symptoms.
*Names and voices have been changed to protect the privacy of interviewees
What side effects did you experience from the Covid vaccine?
Alice: “Everything I used to fear about my condition came back, especially the emotional symptoms, and I’d forgotten how bad they could be.”
In what ways has this affected your day-to-day life?
Zainab: “I think because periods are an accepted part of life for many women, we forget that a disruption to them can really mess with your system.
“As well as physical symptoms it was also just the hassle of having to think about taking tampons with me wherever I went, just in case and not wearing anything too pale a colour.”
What kind of responses did you receive from any medical professionals you spoke to about your symptoms?
Zainab: “I’m pretty okay raising medical concerns and talking about my body so I think for someone less confident, that kind of response would have been awful, especially when it’s about something so personal like a period.”
These women are not alone in feeling that women’s health concerns are underplayed and under-researched and it seems the problem is much wider than the COVID-19 vaccine.
Polycystic ovary syndrome (PCOS) and endometriosis have been discussed more widely in recent years. PCOS affects how the ovaries work and can cause irregular periods, difficulty getting pregnant, excessive hair growth and more. Endometriosis is a condition where tissue similar to the lining of the womb starts to grow in other places, including the ovaries and fallopian tubes. It can cause severe pain, difficulty getting pregnant, and heavy periods.
Those who suffer from the conditions say much more needs to be done to end the silence and taboo around them, and around women’s health more broadly.
Callie Mole

Photo from Callie Mole
Photo from Callie Mole
Callie, 26, has been diagnosed with both PCOS and Endometriosis, she has lived and worked in South London most of her life. We spoke to her about her diagnosis journey and how the conditions affect her life day to day.
For those facing similar issues Callie recommends support groups; Endometriosis UK has links to mailing lists and Facebook groups in each region and she also recommends Stuff That Works, a website which pools information from members to work out which treatments work best for different health conditions.
Vivien Szincsak

Photo from Vivien Szincsak
Photo from Vivien Szincsak
Vivien, 29, has spent the last few years searching for answers after experiencing abnormal bleeding, pain, and hormonal imbalance. Passed between doctors in the UK, and in Hungary, she was given contradictory treatments for a diagnosis of PCOS and potential endometriosis. It was only four months ago that she finally received the surgery she needed for a uterine fibroid diagnosed in January 2020.
Vivien recommends the book The Period Repair Manual, by Lara Briden for all those who menstruate.
Watch the video below to hear Vivien and Callie talk more about their experience of the gender health gap and living with PCOS, endometriosis and uterine fibroids.
TW: Brief mention of suicide
Callie and Vivien's stories
Callie and Vivien's stories


Moves for change
At the end of last year the government set out their vision for a UK Women’s Health Strategy after research found widespread dissatisfaction with the way women’s health was approached.
The research resulted in recommendations in two key areas: to provide education and reliable information on women’s health and improve access to services for support and advice about women’s health.
The government are appointing a Women’s Health Ambassador to raise awareness on the importance of women’s health and support the implementation of this strategy.
Ginsburg Women’s Health Board (WHB) is an independent advisory board which aims to remove the gender health gap in the NHS for women of all intersections. They are working alongside the UK government and challenging them to improve health equality.
Mika Simmons, co-founder of Ginsburg WBH, alongside Nimco Ali OBE, is a British filmmaker, actress and founder of The Happy Vagina, a global community empowering women to talk more openly about gynaecological, sexual and reproductive health.
She also co-founded The Lady Garden Foundation, a national women’s health charity that raises awareness for gynaecological health.
I spoke to her about what steps we should be taking to reduce the gender health gap and why she thinks it has taken so long:
What motivated you to get involved in championing women's health and why do you think it's so important?
"I feel it’s extremely important for those of us who have a public platform to use it for good, to make change. My commitment to change in women's health started after losing my Mum to Ovarian Cancer.
"After her death, and for the longest time I regurgitated the message that this specific cancer “is a silent killer” due to its lack of symptoms and late diagnosis. Then via my work as host of The Happy Vagina podcast I began to understand through experts and research that actually we have a vast gender health gap.
"Amongst other gender health discrepancies, the ovaries were actually only “discovered” in the 19th century.
"Women's bodies have been ignored and overlooked since the beginning of western medicine so to effect change in the specific diseases, like ovarian cancer, we need to dramatically close the gap in understanding."
Why do you think so many of the issues involved in women's health are still so taboo and under-represented?
"Because the modern western health care system was created, and then led, by men since its creation.
"And those men have assumed a male body as the default, with a vast negligence to the Anatomy and Physiology of a woman’s body.
"I believe that with the amount of knowledge and excellent science we have today, to continue to ignore this discrepancy would be a form of violence against women."
How do you think we can reduce the gender health gap while paying attention to the variety of needs for women across all intersections?
"It should begin with better education for the individual and much more woman-specific medical research from the experts.
"Then, stop gaslighting women by suggesting symptoms are psycho emotional.
"Then, ideally, put a system in place to immediately fast track women's health conditions after a GP appointment to appropriate experts."

Photo by Nick Fewings on Unsplash

Photo by Duncan Shaffer on Unsplash
Image credits: photo of Covid-19 vaccines (by Daniel Schludi on Unsplash); photo of period products (by Natracare on Unsplash); your body belongs to you (by Mika Baumeister on Unsplash) photos of Callie Mole (Callie Mole); photos of Vivien Szincsak (Vivien Szincsak); white arrow (by Nick Fewings on Unsplash)


