Gender bias in healthcare
How men being the default in medicine is putting women's lives at risk

For generations women have lived in a society where the healthcare system is designed for men by men.
Recent studies have shown how this impacts women throughout their life.
The Office for National Statistics (ONS) released a report in September 2020 that showed life expectancy at birth in the UK in 2017 to 2019 was 79.4 years for males and 83.1 years for females.
However, despite living longer than men, women spend a quarter of their life in ill health or disability in comparison to men who spend a fifth.
This is the result of ‘male by default’ trials. Women are underrepresented in clinical trials which creates worrying gaps in data and understanding.
It is not only in trials that women are underrepresented. Healthcare equipment and PPE is designed for men, putting women who wear it at risk.
Another issue lies in the stigmas and taboos around women’s health, which can prevent women coming forward with concerns. Often, they are ignored, as shown in the First Do No Harm Report published in 2020.





In 2019 Dr Kate Young, a public health researcher at Monash University in Australia was interviewed for the Guardian by Gabrielle Jackson where she discussed her research which uncovered how doctors fill knowledge gaps with hysteria narratives.
“The historical hysteria discourse was most often endorsed when discussing ‘difficult women, referring to those of whom treatment was not helpful or who held a perception of their disease alternative to their clinician,” said Dr Young.
During her first pregnancy Dr Amina Ahmed, a general practitioner from Bradford, Yorkshire was training in obstetrics and gynaecology, which is the field of medicine concerned with the care of pregnant women, their unborn child and the management of diseases specific to women.
Dr Ahmed was unwell, vomiting eight to ten times a day. Her male consultant was less than sympathetic and accused her of exacerbating her sickness, even though she could provide notes from doctors confirming the illness.
She had to get a reference from her consultant of six years during her A&E training to verify that this was out of character.
It was only three years later, when she was pregnant with her second child, that it was confirmed she had an undiagnosed tumour.
Her unborn baby had been sat on the tumour which was releasing adrenalin and making her sick.
Even being a medical professional, Dr Ahmed’s concerns were not taken seriously.
Taken to hospital during her second pregnancy for severe abdominal pain, as she lay on a hospital bed, she experienced excruciating pain in her hip.
Dr Ahmed told me: “I had this pain, it was not like anything I’d had before.
“I called the midwife to help me turn over and she looked at me and said: ‘We have lifting and handling procedures, you will have to do it yourself’.”
Dr Ahmed lifted herself and turned herself over, as she did so, she immediately vomited.
After going back to sleep for a while she woke up in pain again. Calling the same midwife into the room she asked her to stand at the end of the bed in case she fainted as she lifted herself up.
A trainee who was stood with the midwife stepped forward to assist at which point the midwife said, “No she has to do it herself.”
The following two days Dr Ahmed remained in the hospital under observation, the doctors could not figure out what was causing the pain. It was only when they noticed her blood count drop from 12.8 to 4, that they realised something was very wrong.
It was assumed, that as a woman, she was anxious, and this was causing the drop.
Dr Ahmed noted that if she was anxious and hyperventilating her oxygen saturation would increase not decrease.
After being rushed into an operation she woke up in ICU and a surgical consultant informed her that when they had opened her up, around two litres of blood had poured out of abdomen, she’d had an internal haemorrhage caused by turning herself over in the hospital bed two days before.
She had lacerated her liver.
During the Covid-19 pandemic women on the front line have been left vulnerable due to sexist PPE equipment.
Although more than three quarters of the NHS workforce are female, seven out of ten women did not feel protected.
Some companies that distribute face masks design them to the European Standard, one of the requirements is that the mask should be tested on ten clean shaven faces.
This is not a new issue. The gowns for medical staff have always been too large and can become a tripping hazard.
The one size fits all mentality is putting women’s lives at risk as it is based off of “reference man”.
Reference man is 25-30 years old, he is white, and he weighs 70kg and yet he represents the entire work force.
Dr Helen Fidler, deputy chair of the British Medical Association (BMA) UK consultants committee told the Guardian: “Women’s lives are absolutely being put at risk because of ill-fitting PPE.
“We know that properly fitted PPE works, but masks are designed for a male template, with the irony being that 75% of workers in the NHS are female.”
However, it is not just PPE that does not fit, it is training equipment too.
Mannequins that are used to teach CPR are based off of a man’s build and body, they do not include breasts.
While the breast tissue will move, it is much more difficult to perform CPR on a woman, than on the dummy that first aid training is taught off.
This has a detrimental impact on women who are less likely to receive bystander CPR than men.


Prior to a guideline issued in 1994 by the US National Institutes of Health (NIH) women had been excluded from early study of most drugs.
This had a huge impact on the information about the effects of drugs in women and in 2005 it was reported that eight out of ten prescription drugs were withdrawn from the US market because of women’s health issues.
In her TED Talk Alyson McGregor discusses why medicine often has dangerous side effects for women.
Everyday drugs such as Ambien and aspirin were only ever tested on men and their side effects on women can be dangerous and sometimes deadly.
These drugs have to go through rigorous trials before they are available for a doctor to prescribe them to a patient. They are tested on cells, animals and humans before their approval process.
However, the reason their impact on half the population goes unnoticed after millions and billions of dollars are spent is being those cells and animals were male and the human clinical trials were done almost exclusively on men.
It was not until 2014 that the NIH began to acknowledge the issue of male bias in clinical trials.
In 2016 the NIH mandated that any research money it granted had to include female animals.
After World War II there were guidelines put into place to ensure people were not a part of medical trials without their consent.
These guidelines also said that in order to protect women of a childbearing age from any side effects of these medical trials, they were not allowed to participate.
This also made these studies much more cost effective as men’s bodies are fairly homogeneous.
Women have constantly fluctuating hormones, especially those using hormonal contraception who must be considered as a separate group for the purpose of analysis as stated by Anita Holdcroft in her paper: Gender bias in research: how does it affect evidence based medicine?
Holdcroft goes on to say: “A study in Sweden from 1997-1999 investigated why researchers excluded women from clinical trials.
“The scientific reasons for excluding women were a lack of physiological data, repeat of studies that had previously used only men so as to obtain comparable data, and the economic costs of research in women.”
In 2007 the Society Women’s Health Research published guidelines advising that research into sex differences should include different hormonal states. This methodology had the potential the quadruple medical research grant costs.

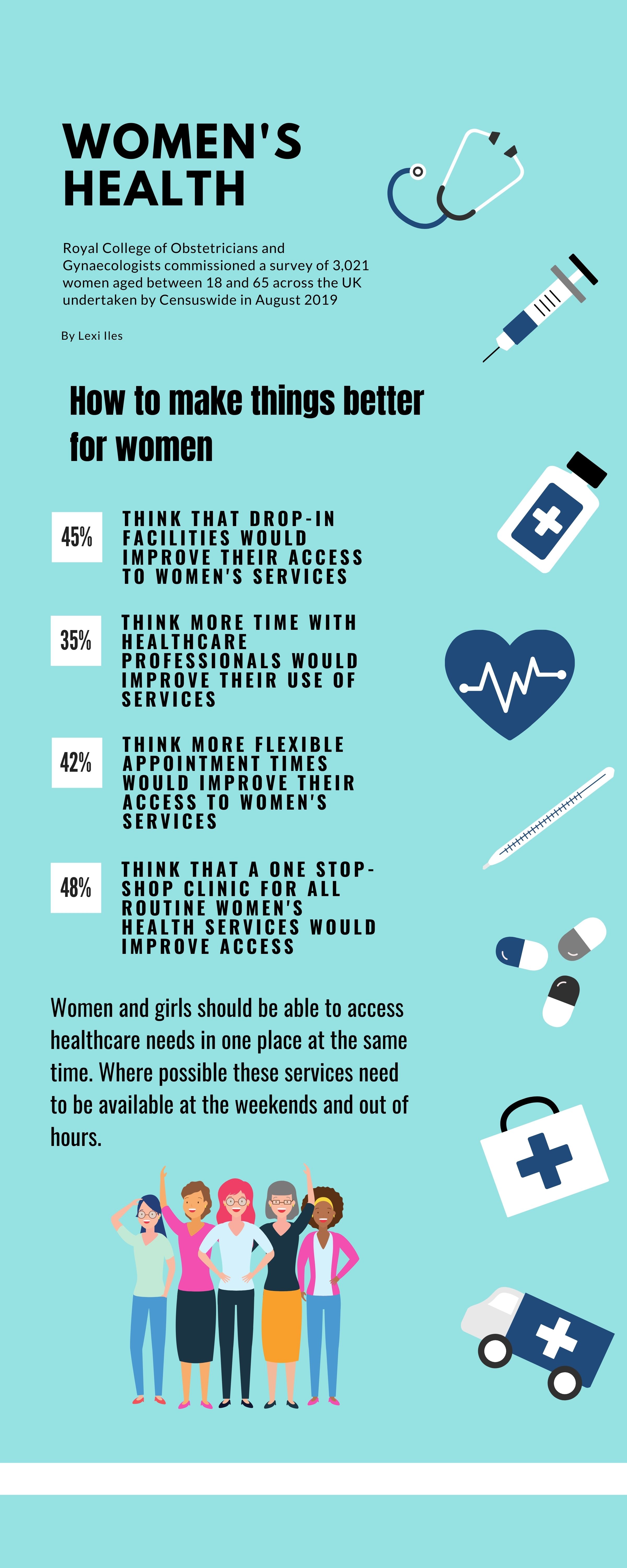
Earlier this year, in the UK, the government made a call for evidence seeking the views of women to help inform the development of Women’s Health Strategy.
The government has recognised that the underrepresentation of women can lead to poor advice and diagnosis which can result in a worse outcome.
Hopefully, steps like this will help diagnose women with conditions such as endometriosis, which affects 190 million women, of reproductive age, globally but takes eight to ten years in the UK to diagnose.
The Call for Evidence focused on six core themes:
1. Placing women’s voices at the centre of their health and care
2. Improving the quality and accessibility of information end education on women’s health
3. Ensuring the health and care system understands and is responsive to women’s health and care needs across the life course
4. Maximising women’s health in the workplace
5. Ensuring research, evidence and data support improvements in women’s health
6. Understanding and responding to the impacts of COVID-19 on women’s health
However, Doctor Fiona Macmillan, a general practitioner who set up and runs a sexual health practice in Wigan believes that women access medical services better.
Doctor Macmillan said, “Women come forward I think because contraception, for young women, is their responsibility.
“They approach sexual health services, family planning and then have children who they bring in for appointments.
“So, women are much more open to accessing medical services than men."
She believes that things have improved since she started training in 1985 and that while there is still a delay to diagnosis for conditions such as endometriosis and polycystic ovaries, it is much better than it was.
Doctor Macmillan believes that by allowing doctors, who have specialist knowledge, to see patients outside of their own clinic would improve health services not just for women but across the board.
"If GPs could refer their patient to a GP within the area who has a specialist knowledge or interest, that way you get little clusters of special interest doctors working for the whole district," said Doctor Macmillan.
In doing this she believes it would prevent some patients being sent to secondary care services and ease the pressure.