Living with Premenstrual Dysphoric Disorder
Unheard, Misdiagnosed and Suicidal Ideations

Introduction
"When PMDD hits, its like I'm watching myself disappear. I feel numb, disconnected and I can't believe I ever felt good. Every month I think, there's no way it'll be that bad again, and then it hits - and it is."
Williams is one of millions of people across the world suffering from Premenstrual Dysphoric Disorder.
In its simplest terms, the disorder is characterised as an abnormal response to hormonal fluctuations during a person's menstrual cycle.
Those hormones manifest intense psychological and physical symptoms within an individual, endangering their emotional stability, their relationships, career, and in some cases, their own life.
The cyclical nature of the disorder often paralyses individuals into an acute state of depression and anxiety on a monthly basis, which can last a lifetime if it remains undiagnosed.
Yet the effects of PMDD linger far beyond the designated hormonal period of the menstrual cycle.
The repercussions persist into the rest of their daily lives, as those affected are left to pick up the pieces of the aftermath.
While there are signs of growing medical awareness towards the condition, a significant gap remains in the education of health professionals on women-specific illnesses.
This leaves many women misdiagnosed, unheard and left to cope with these conditions on their own.
Approximately 31 million women and girls across the world are diagnosed with Premenstrual Dysphoric Disorder, according to a University of Oxford study.
In the UK alone, that’s approximately 824,000 people, of which 275,000 will attempt suicide, according to the University of West Scotland.
That's one in three.
And these statistics only include the women who have received a diagnosis.

Meet Phoebe Williams: The CEO of the UK's first PMDD charity
“There are too many people suffering in silence. We want to change that.”
Phoebe Williams
Image credit: Phoebe Williams
Image credit: Phoebe Williams
Williams is a 28-year-old Londoner who wears multiple hats: she is the Fundraising Manager at the British Heart Foundation and the founder of The PMDD Project - the UK's first charity dedicated to supporting people with PMDD - all while living with the disorder herself.
Registered in 2024, Williams initiated the PMDD Project after years of navigating the disorder alone, experiencing regular dismissals and misdiagnoses from UK general practitioners.
The founder said:“I'd describe myself as a warm, outgoing person who deeply values my friendships, my family, and my relationship.
"I've always been the bubbly one in the group - creative, passionate and full of energy - at least when I'm not in the luteal phase of my cycle, which is a different story altogether.”
Through the PMDD Project, Williams is hoping to impose legislative and social change in the awareness and research towards the debilitating condition.
She said: "The mission is simple but urgent: to provide practical resources, support, and awareness for people with PMDD so that they feel less alone and more empowered.
"We're also working to push PMDD up the agenda in healthcare, workplaces, and policy - because change doesn't happen unless we demand it."
What is PMDD?

Premenstrual Dysphoric Disorder is characterised as a more severe form of Premenstrual Syndrome (PMS), where intense psychological and physical symptoms arise across the luteal phase of the period cycle - that’s the two weeks before a period begins.
The severe symptoms are recognised as an abnormal reaction to normal hormonal changes throughout the menstrual cycle.
Dr Vikram Talaulikar, Specialist in Reproductive Medicine, expanded further on the effect of such hormonal fluctuations for individuals with the disorder:
For Williams, the luteal phase of her period has a transformative influence on her personality.
She said: "I'm honestly like two different people. Outside of the luteal phase, I'm happy, bubbly, confident, full of love and energy. I have so much empathy and joy.
"When PMDD hits, it's like I'm watching myself disappear. I feel numb, disconnected and I can't believe I ever felt good."
Psychotherapist Emily Holloway, who specialises in clients with PMDD, offered insight into the behavioural changes a person can undergo while experiencing the luteal phase.
Holloway used the hypothetical 'mug' scenario - a visual tool to depict the transformative effect of the hormonal phase to first-time clients.
What are the symptoms?

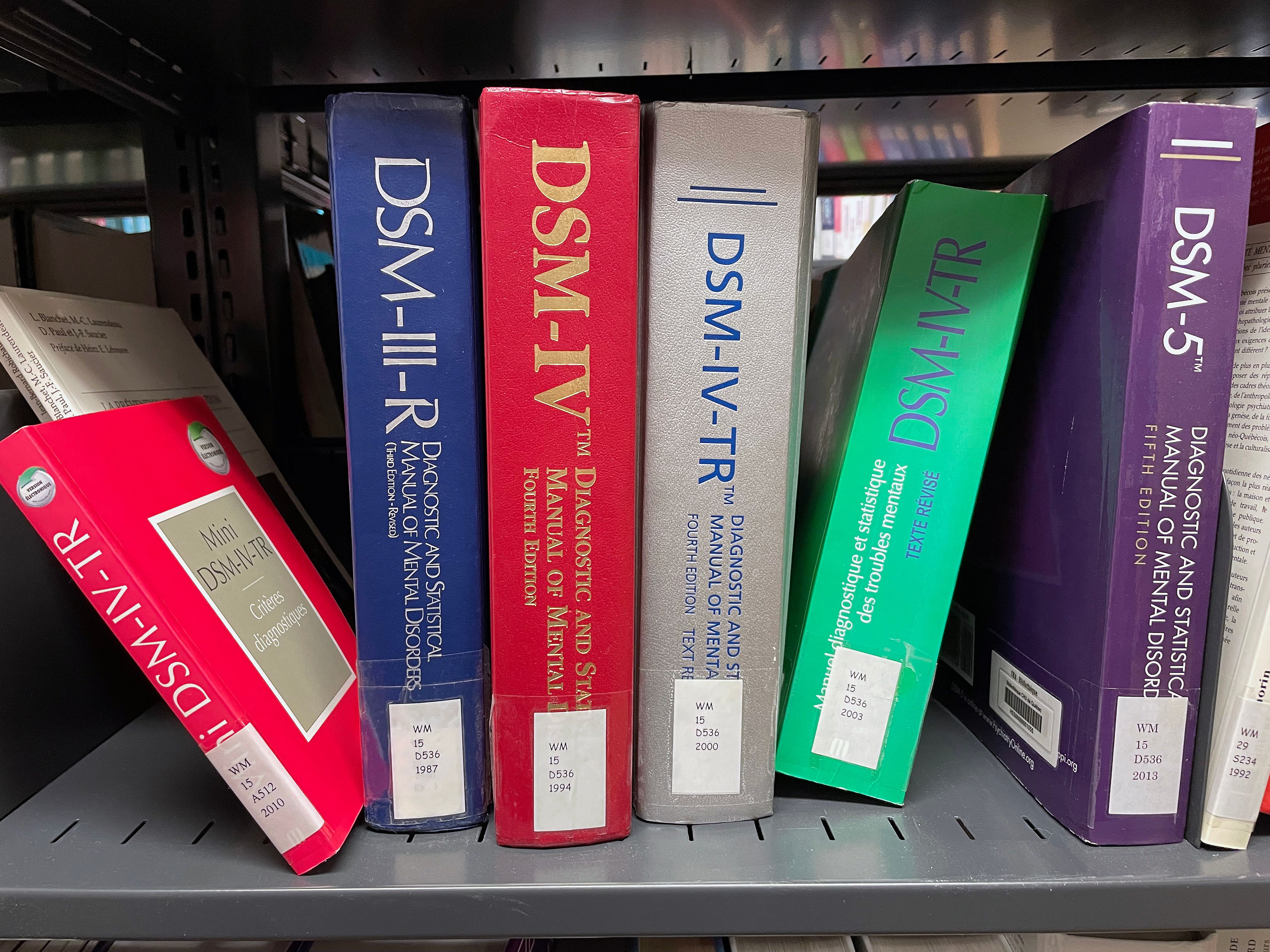
PMDD is defined in the Diagnostic and Statistical Manual of Mental Disorders (DSM), as occurring when a woman suffers from at least five distinct psychological premenstrual symptoms.
The symptoms include:
- depressed mood
- emotional lability
- irritability and anger
- poor concentration
- tension and anxiety
- loss of interest in usual activities
- altered eating habits or food cravings
- disturbed sleep patterns;
- lethargy and fatigue
- feeling overwhelmed or out of control
- physical symptoms such as headache, breast tenderness, weight gain and feeling bloated.
Dr Talaulikar outlined the numerous symptoms an individual may undergo, placing particular emphasis on the potentially life-threatening impact of the psychological symptoms.
Williams first encountered PMDD symptoms at 16 years old, but at the time, she brushed them off as nothing more than the typical teenage experience:
"I noticed how extreme my emotions became in the lead-up to my period - specifically this irrational rage that didn't match with what was happening around me.
"At the time, I just thought that I was a moody teenager."
However, as her symptoms surpassed the years of adolescence, she began to realise that the drastic changes to her behaviour may be something different entirely.
"By the time I was living with friends at university, it became clear something wasn't right.
"I'd swing from being really happy to crashing into this dark, low place, feeling depressed and hopeless.
"I remember thinking, "Why am I reacting like this and my friends aren't?"
"By 22, things had escalated to the point of experiencing suicidal ideation and I knew that I desperately needed help."
Psychotherapist Holloway spoke on the emotional turbulence that people can undergo during this critical stage:
Once the hormonal phase subsides, the symptoms alleviate.
During this transition, Holloway described the sense of relief which may emerge as the effects of the luteal phase begin to cease:
"All the colour floods back in. People describe it as they can 'suddenly see the flowers', everything has clear lines again.
"Those feelings of not wanting to exist are flushed away with delight, because you do exist."
While the symptoms may abate, the effects of the luteal phase linger into people's daily lives, as they are left to face the repercussions.
The PMDD specialist dived into examples on the damage caused by a single hormonal phase:
For Williams, PMDD symptoms affect every facet of her life:
"Socially, I tend to hide away during the luteal phase because I'm too anxious and low to be around people.
"In relationships, I get really insecure and there's often a huge drop in sexual intimacy. I just shut down emotionally and physically.
"Professionally, it's been brutal at times. I've had to work through symptoms that make it nearly impossible to concentrate or engage with others."
For many, feelings of depression are exacerbated by the emotional, social, physical and professional setbacks encountered throughout the debilitating hormonal period.
Dr Talaulikar said: "It's a vicious cycle.
"As you experience the changes caused by PMDD, you automatically close down.
"You're avoiding social circumstances, you're going out less, your work suffers, and sometimes you're also not getting help.
"Staying in your own shell then adds to further feelings of low mood and depression and impacts your quality of life."
A brief medical history

On medical record, PMDD has a fairly recent history, introduced in writing as the Late Luteal Phase Dysphoric Disorder in 1987 in the Diagnostic and Statistical Manual of Mental Disorders (DSM) by the American Psychiatric Association.
The DSM is a globally recognised handbook used by healthcare professionals in the United States and across the world, including the UK.
The GPnotebook for example, an online clinical resource for UK general practitioners (GPs), refers to the DSM as a strict guideline for the diagnosis of PMDD.
However, it was not until 2013 that the condition was officially recognised as a mental illness by the fifth edition of the DSM.
Conversely, PMS is not classified as a mental disorder in the manual, unlike PMDD.
Image credit: H_Ko
Image credit: H_Ko
Image credit: Ivan Samkov
Image credit: Ivan Samkov
Image credit: Pascal Huot
Image credit: Pascal Huot
The Increased Risk in Suicidal Ideations and Self-Harm

From harrowing personal testimonials to a large pool of international studies, it is widely accepted that women with PMDD are at an increased risk of having suicidal ideations.
Furthermore, women with the disorder were almost four times as likely to exhibit suicidal ideation.
Williams is one of the many women who continues to live with the weight of creeping suicidal ideations:
"Throughout it all, a sense of deep self-doubt has remained constant.
"These days, my symptoms are rooted in apathy and depression.
"Sometimes, suicidal ideation creeps back in, though thankfully that's not constant."
Researchers from the UWS outlined that out of the 824,000 individuals with PMDD in the UK:
593,600 experience suicidal ideations - that's 7 out of 10 women.
412,000 will self harm.
275,000 will attempt suicide.
In a 2024 Manchester study, 14 women interviewed on their experiences of PMDD symptoms revealed that the risk of suicidal ideations, self harm and suicide attempts is heightened by the delay in receiving a diagnosis.
Unheard and Misdiagnosed: The painful female experience at the doctor’s office

At present, people with PMDD in the UK visit health professionals for 4 to 14 years before receiving a correct diagnosis.
William's experience at the doctor's office was no exception to the rule:
"I spent years going back and forth to GPs and was constantly told it was 'just PMS' or that it was down to my lifestyle.
"One GP told me I was being dramatic. Another suggested I might have bipolar disorder because of my mood swings - without ever once asking if my symptoms followed a menstrual pattern.
"No one connected the dots, and I was made to feel ashamed and hysterical."
Women being the recipients of a misdiagnosis is not an exclusive experience to those with the premenstrual disorder, and is reflective of a wider international crisis of sexism strife within the health industry, where a single misdiagnosis could be fatal.
Currently, women are 50 percent more likely than men to be given an incorrect diagnosis following a heart attack, according to the British Heart Foundation.
In a survey of 500 women who have experienced an incorrect diagnosis, Higgs LLP uncovered that one in four women surveyed had a gynaecological or female-specific illness misdiagnosed.
These included Polycystic Ovary Syndrome (PCOS), period pain, ovarian cysts and endometriosis emerging as the most frequently misdiagnosed condition.
Within the same survey, one in four women reported being wrongfully prescribed pain medication to suppress their symptoms without addressing the underlying cause.
Image credit: Svyatoslav Lypynskyy
Image credit: Svyatoslav Lypynskyy
For Psychotherapist Holloway, the root cause for rushed dismissals and misdiagnoses was abundantly clear:
"The obvious answer is medical misogyny. We have a patriarchal medical system.
"As people who identify as women, we are dismissed, constantly.
"I work constantly with clients that have experienced medical professionals tell them 'it's just in your head', or 'everyone goes through this.'"
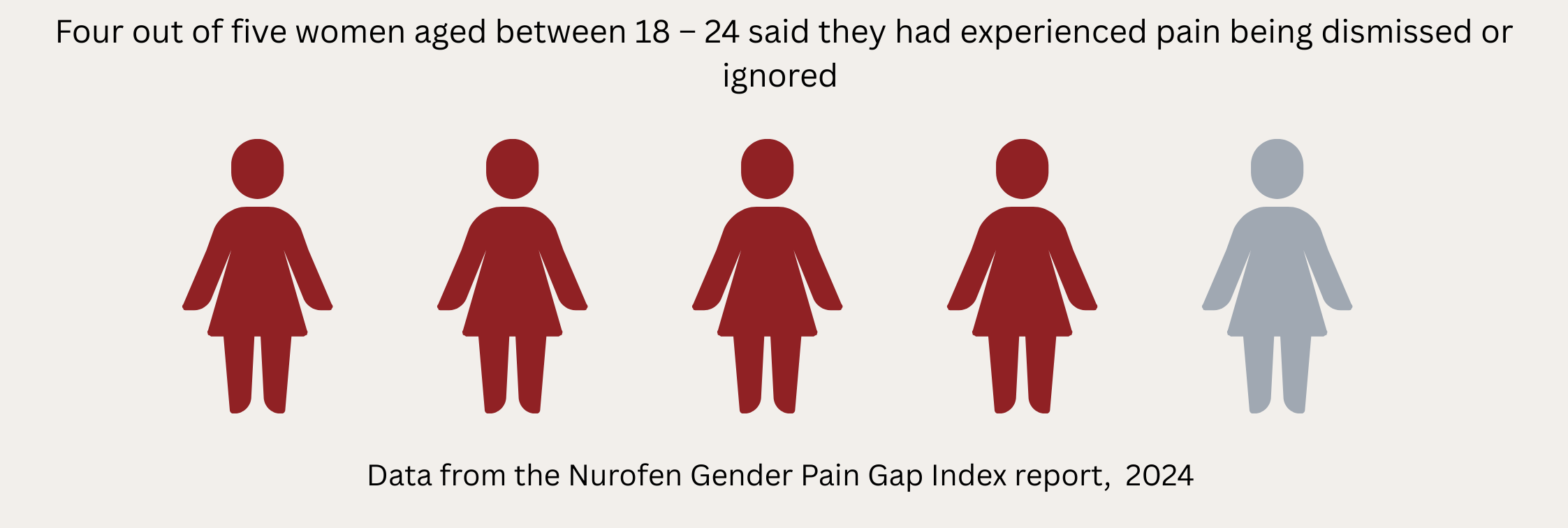
A gendered disparity between women and men’s experiences of pain dismissal by healthcare professionals was unveiled by a Nurofen report in 2024.
The report measured a gender pain gap of seven percent, as 81 percent of women aged between 18 and 24 said they had experienced pain being dismissed or ignored, compared to 73 percent of men.
The glaring lack of awareness in women-related illnesses often results in women reporting misinformed dismissals, medical gaslighting and perceived 'female hysteria'.
As a result, many healthcare professionals fail to follow the appropriate diagnostic process for PMDD.
The correct path to a diagnosis requires tracking symptoms daily across at least two full menstrual cycles to confirm the cyclical nature of the condition.
The disorder is then treated by gynaecologists.
Dr Talaulikar noted that failure to follow the correct diagnostic process among health professionals was far too frequent an occurrence, extending to GPs, hospital specialists and even some gynaecologists.
After years of being misheard, Williams was forced to take matters into her own hands to ensure a diagnosis.
The PMDD Project Founder said: "Eventually, I discovered PMDD myself through relentless online research.
"I went back to the doctors, spoke to a new GP, and told him 'this is what I have'".
The GP in question had never heard of the disorder, but after taking the time to research it, Williams was diagnosed the following day.
But the battle didn't end there.
Williams continued: "Since then, I've seen gynaecologists, but even they often have to google PMDD during the appointment.
"There's just such a lack of knowledge across the board."
The high risks of misdiagnoses among healthcare providers naturally demands the question for women with PMDD - who should I go to for an informed diagnosis?
In a global survey regarding the premenstrual disorder, American researchers measured the efficiency levels of varying health care providers based on the experience of the patient.
These included GPs, psychiatrists, gynaecologists and psychotherapists.
Patients rated health care providers in three areas:
1. Interpersonal factors
2. Awareness and knowledge of PMDD
3. Whether the patient was asked to track symptoms daily
In regards to interpersonal factors, psychotherapists were rated the highest by PMDD patients.
Gynaecologists and psychiatrists were rated the highest for the awareness and knowledge of the condition, unlike GPs.
And finally, gynaecologists were most likely to ask patients to track their symptoms daily compared to other healthcare providers.
Reproductive Medicine Specialist Talaulikar faulted the minimal retraining on new PMDD research among GPs:
Victims of incorrect diagnoses were not the only ones to voice their concerns on the lack of awareness among health professionals in regards to female-specific conditions.
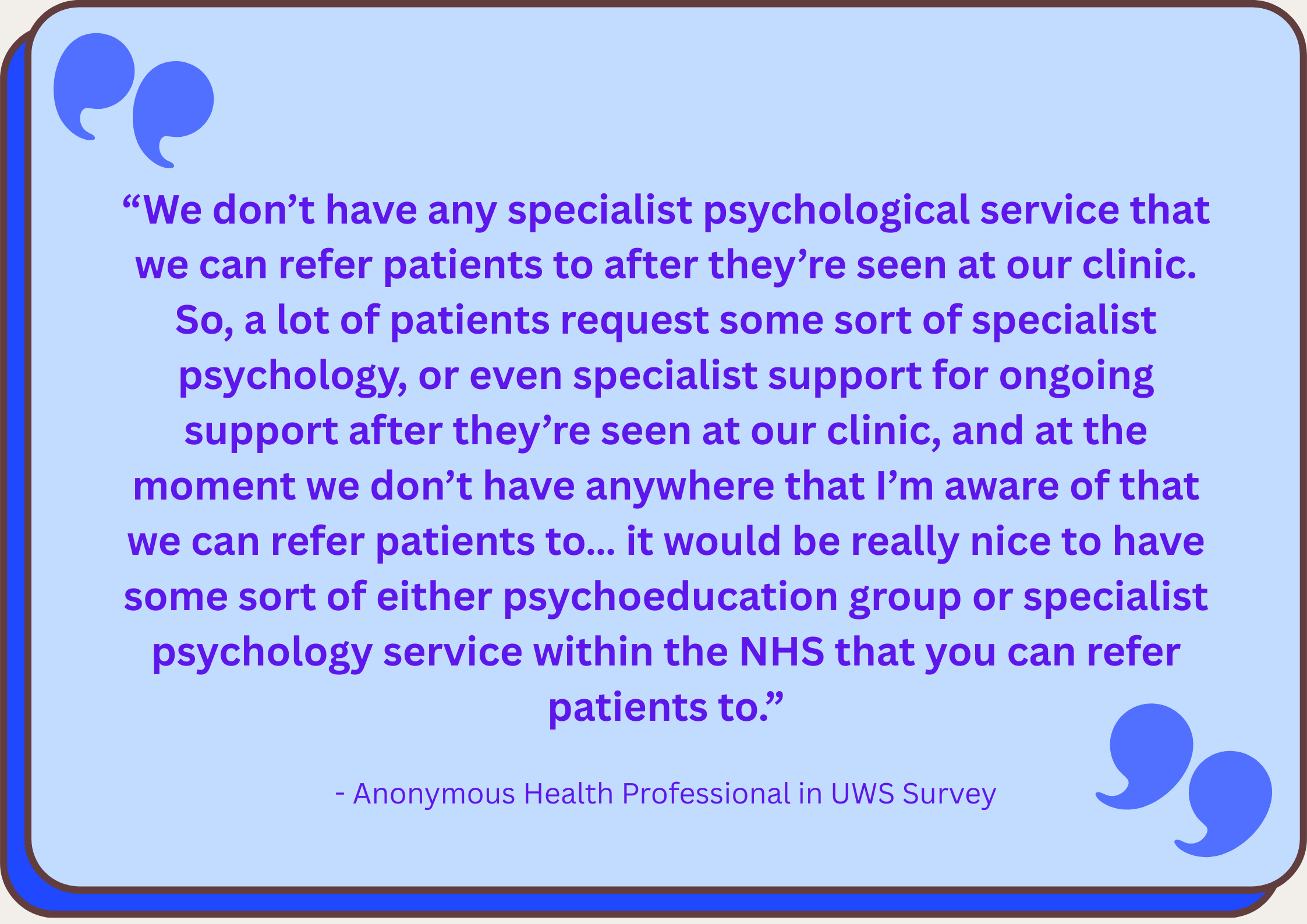
Members of the health industry themselves aired their frustrations on the systemic boundaries of the NHS and the limited resources available to cater to women with PMDD in the UWS report.
This claim was further reinforced by emergency crisis personnel working in suicide and self-harm prevention, who described the challenges posed in supporting people with PMDD with limited options, particularly if they, nor the patient have recognised the condition themselves.
Misdiagnoses and dismissals can also arise as PMDD often falls between the domain of gynaecology and psychiatry.
The UWS report concluded that the current groundwork on the best approaches for psychiatric support is insufficient, as people with the condition may require coping skills which span a lifetime.
Treating PMDD

After receiving a PMDD diagnosis, it opens the doors for the next logical step: seeking treatment.
But, for Williams, receiving her long-awaited diagnosis arrived with mixed emotions:
"Honestly, it was both liberating and a bit devastating."
"On one hand, it was a huge relief - it was good to put a name to my symptoms, to know I wasn't being dramatic and I wasn't broken.
"But on the other hand, there's this realisation: great, I've got this thing now - and there's no cure.
"Still, overall, I'd say it was validating and certainly life-changing. Once you have a name for it, it's easier to seek support, communicate your needs, and stop blaming yourself."
While the diagnosis may offer clarity, it also presents a new challenge: identifying the most suitable course of treatment.
Specialist in reproductive medicine, Dr Talaulikar, detailed the array of options one can be presented with to treat PMDD:
However, much like obtaining a diagnosis, the path to effective treatment can be unpredictable, often dependent on the level of awareness and expertise of the doctor consulted:
For Williams, it was once again the information she sought outside the doctor’s office that proved most influential in helping her understand her PMDD symptoms.
She said: "Doctors tend to offer two options: antidepressants or hormonal contraception.
"That's pretty much it. It's frustratingly limited.
"I personally can't take hormonal contraceptives - it makes me feel worse because I'm already so sensitive to hormonal changes.
"But I did start on SSRIs and they've helped reduce the intensity of suicidal ideation, which is no small thing.
"That being said, the biggest changes have come from understanding my cycle and building a lifestyle that supports me throughout it.
"I've worked hard to figure out what triggers me and what helps - things like nutrition, movement, boundaries, rest, and creative outlets.
"Unfortunately, this kind of holistic, personalised support is rarely offered by medical professionals. You have to become your own expert."
Psychotherapist Holloway is one of the few specialists offering holistic support tailored specifically to people with PMDD.
The PMDD specialist said: "I work in a mix of person-centred, existential, solution-based approach."
Holloway emphasised the importance of exploring the underlying emotions that the disorder may exacerbate.
She said:"PMDD likes to come in and find where you are at your most vulnerable.
"Whether it be unprocessed traumas or unprocessed experiences, if we can try and unpick that, once PMDD comes, it will have less stuff to poke at."