Pain and IUDs
A call for change
By Hannah Roberts

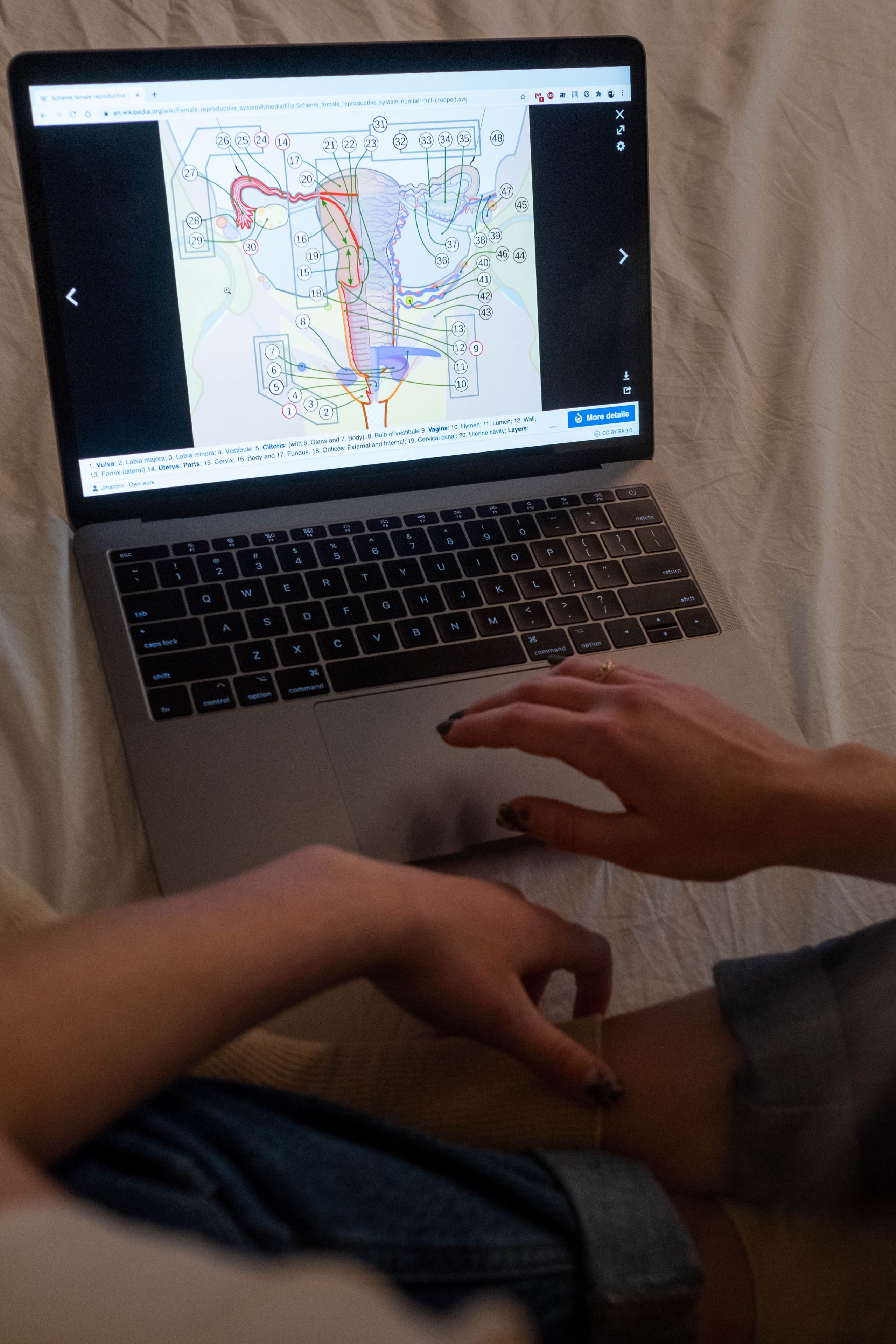
IUD procedures
In 1909 the first intrauterine device was invented with more being developed throughout the 1920s.
They only started to receive widespread use in the late 1950s, when plastic devices were invented.
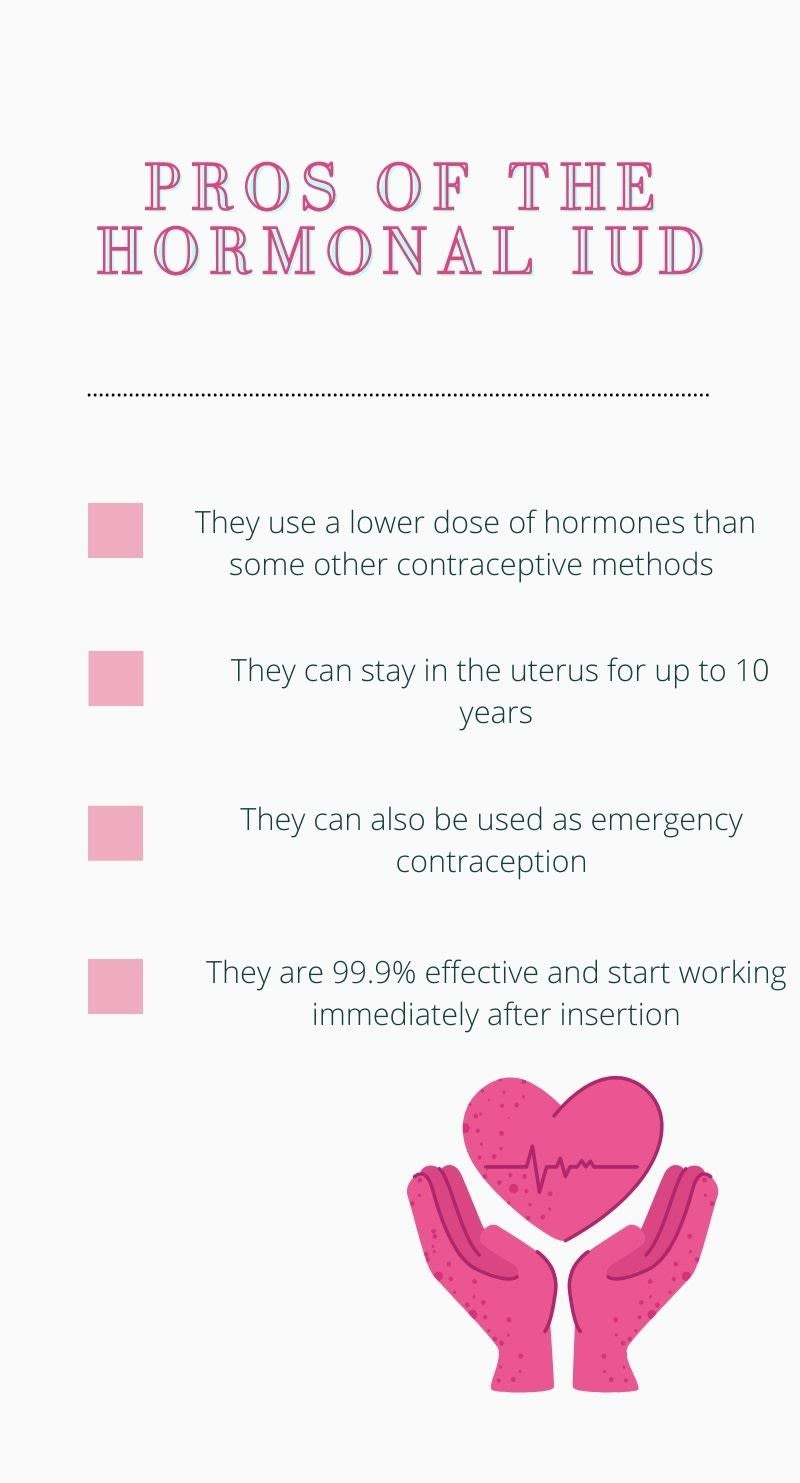
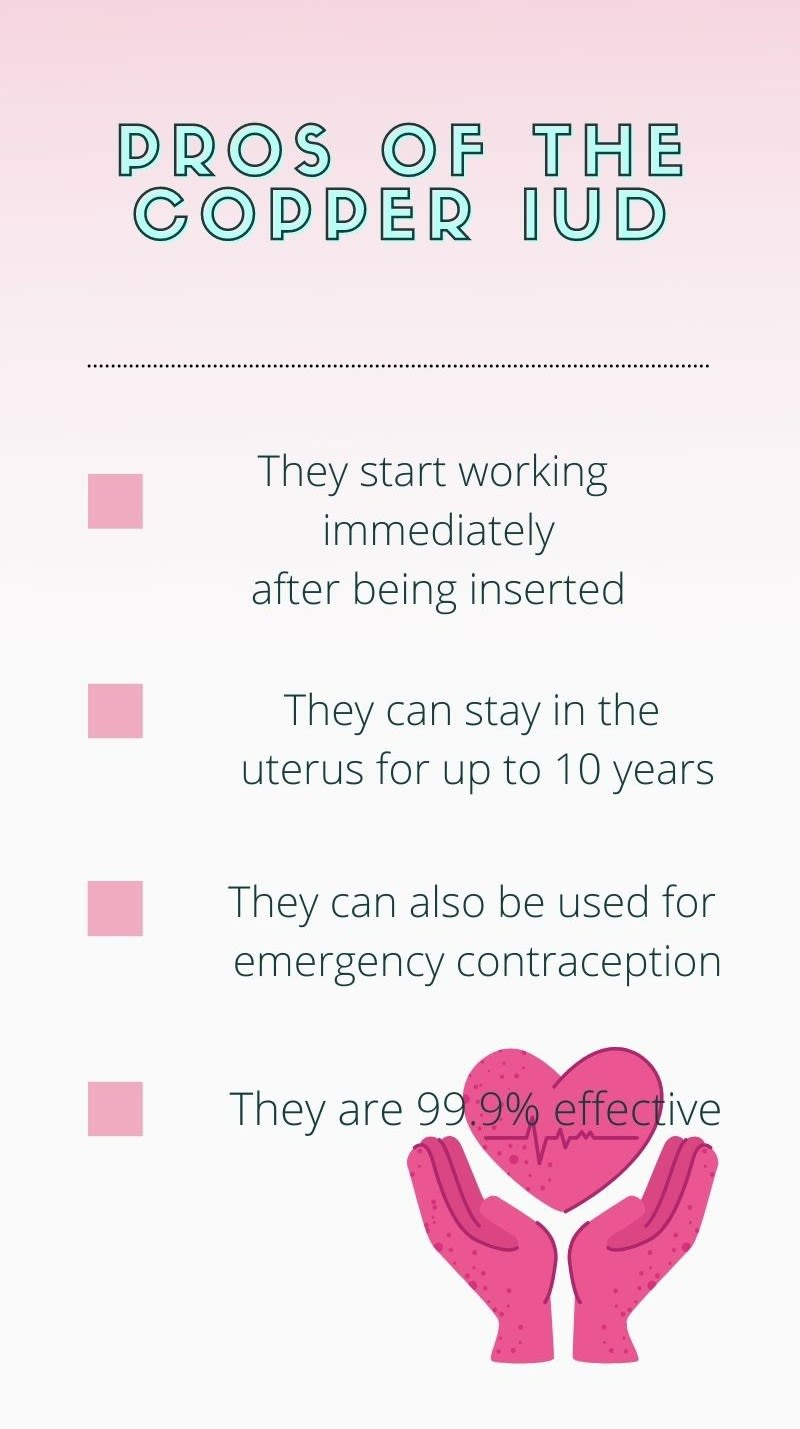
The two main types of IUDs are hormonal and copper. IUDs can protect from pregnancy for around five to ten years and are 99.9% effective. They're inserted through the opening of the cervix and placed into the uterus.
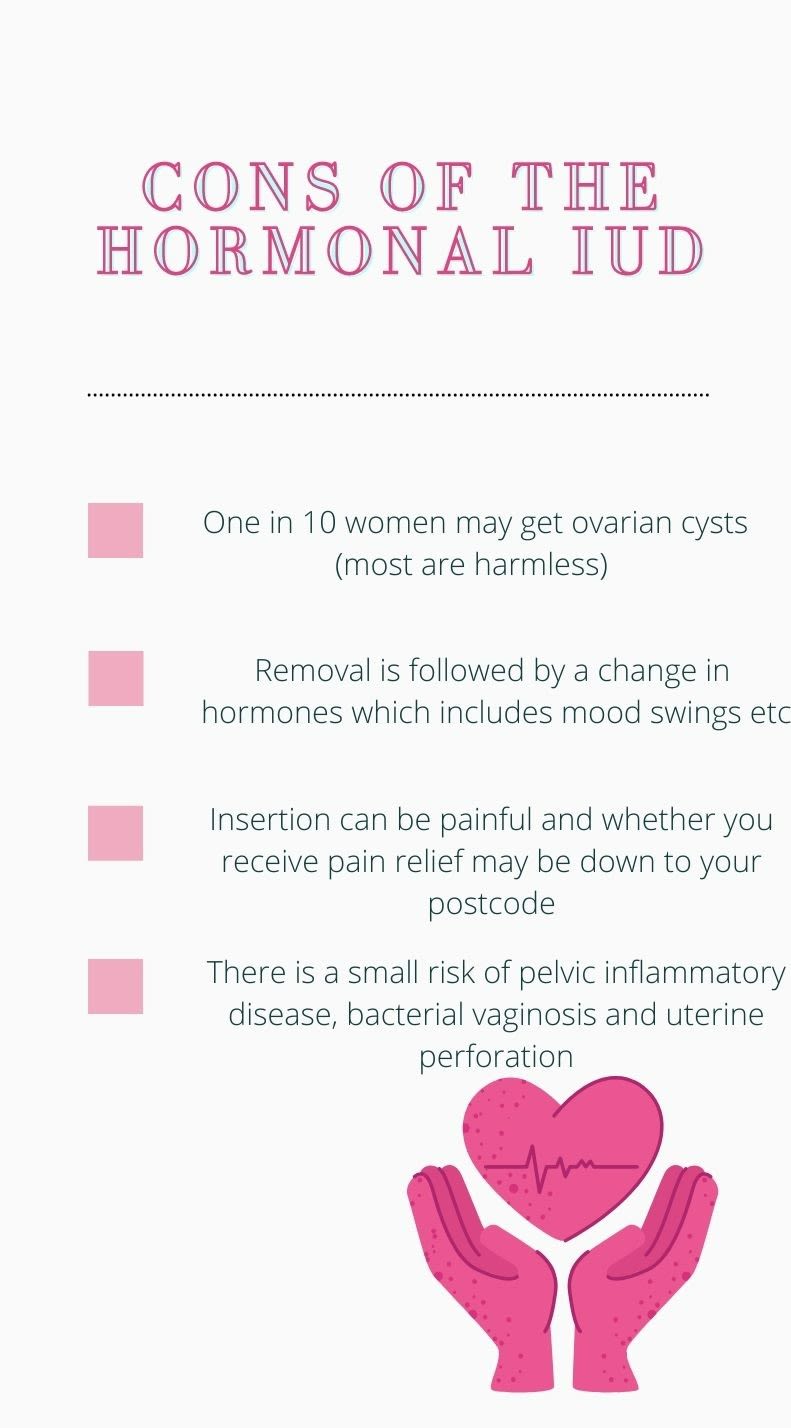
The NHS website says that "having an IUD fitted can be uncomfortable and some people find it painful" but that a local anaesthetic can be used to help. It also says "you may get period-type cramps afterwards" but that painkillers can ease the cramps.
The types of pain relief offered to people during IUD procedures can depend on where they live and whether they go to a specialised clinic.
There isn't a lot of data in the UK illustrating the percentage of people who are in pain during IUD insertions, however, a 2013 study by Human Reproduction Update in the US concluded that only 17% of women who hadn’t given birth before experienced substantial pain.
It also said that: “Women's anxiety about the procedure may contribute to higher levels of perceived pain.” The same study showed that ibuprofen has no significant effect in terms of pain management and there was no group consensus that local anaesthetic provided pain relief either.
The study also noted that there is insufficient data surrounding local aesthetics and IUDs, asserting that most data is derived from patients who’ve experienced hysteroscopies.
A Call For Change
Three months ago Lucy Cohen, 38, started a petition to offer better pain relief at appointments for the insertion of IUDs.
Since then over 32,000 have signed the petition and a wave of people have come forward with their stories about the insertion of their IUDs.
Naga Munchetty recalled the agonising pain on BBC Radio 5 saying:
"My screams were so loud that my husband tried to find out what room I was in to make it stop."
Since creating the petition, Cohen has asked for people to share their experiences.
Out of 1500 people surveyed, 43% of respondents rated their pain as a seven or higher, on a scale of one to 10.
Associated words included: extremely painful, almost unbearable, and excruciating.
Cohen said: “The NHS site says that you should be expecting mild discomfort and that was not the case for me at all. That's why I started a survey and about 1500 completed it. That's when I realized that there’s quite evidently a problem.
"There are people who have told me that the pain is worse than childbirth.
"The responses I’ve had have just been heartbreaking. The FSHR have said that they don’t want people to be put off and that the majority of women find it fine but where’s the data saying the majority of women find it okay?
"What I’ve learned is that people don’t collect data on women's pain. There’s no routinely collected information about these sorts of procedures. There’s zero evidence that over-the-counter medicine taken before an IUD procedure does anything.
"I think women are somehow perceived as being built to take the pain.
“I had no idea I had a tilted cervix, not in my many years of having smear tests and that can be an indication that it will be more difficult to fit an IUD. Nobody put that on my medical records so they didn’t know.
"When I was getting the IUD inserted I was thinking who’s making that horrible screaming noise and it was me.
"I was never told about the potential risk of how much it could hurt and it leaves you feeling like you didn’t consent. If you're told about how it could hurt then you can decide.
"I think in 10 years' time we’re going to look back on how women and people with uterus’ health were dealt with in 2021 and think: I can’t believe people were treated like that in 2021.”
Cohen is calling for better support and pain management for IUD insertions. Specifically, the introduction of gas and air, sedation and muscle relaxants to be used as standard procedure.

Lucy Cohen
Lucy Cohen

Image Credit: Robin Marty, Flickr, 12th November 2018
Image Credit: Robin Marty, Flickr, 12th November 2018

Acknowledgement
On the 22nd of June this year the Faculty of Sexual and Reproductive Health (FSRH) released a statement acknowledging the experiences of women who have come forward to talk about the pain they experienced during IUD insertion.
They also recognised that local anaesthetic should be offered as an option for women.
Dr Diana Mansour, Vice President of the Faculty of Sexual and Reproductive Healthcare (FSRH), said:
“No woman should endure severe pain when having their IUD fitted. IUDs are one of the most effective and acceptable contraceptive methods available to women in the UK.
"I offer pain relief before and, where necessary, during an IUD placement including the use of local anaesthesia. I let women know that they are in control during the procedure and at any point additional pain relief can be given or other options explored such as having the IUD fitted under conscious sedation or general anaesthesia in the local hospital.
"Not all clinics or GP practices offer local anaesthesia. Where this is the case rapid referral to another service should be in place. Ultimately, I want to support women to choose a contraceptive which best suits them.
“The FSRH will share updated clinical guidance on this matter and work with our members to share best practice to ensure women experience the highest standards of IUD care.”
Dr Edward Morris, President at the Royal College of Obstetricians and Gynaecologists, said: “We are calling on the UK government to ensure these experiences are recognised and addressed in the new Women’s Health Strategy for England. We need a healthcare system that is designed to support women and make sure they are listened to, and conversations like this are important in shaping women’s services and research priorities moving forward."
The FSRH also said that they welcome future studies, working with users to optimise the patient experience for individuals choosing IUDs.
In 2013 a study was published by the British Medical Journal Publishing Group which set out to determine how often local anaesthetic was used during IUD insertion by UK health professionals.
They surveyed 129 health care professionals and the results showed that around a quarter of all respondents used local anaesthetic routinely and a quarter hardly ever used it, whilst the remaining half used it sometimes.
The use of local anaesthetic was more prevalent in professionals who worked in an integrated sexual and reproductive health care setting.
The professionals who hardly ever used local anaesthetic were more likely to be working in a GP surgery.
The conclusion was that more professionals should routinely use local anaesthetics during IUD procedures.
At the time the guidance from the FSRH did not recommend routine use of anaesthetic during an IUD procedure but did advise that "pain relief should be discussed with women in advance."
In a statement from 13th July this year the FSRH said: "We recommend healthcare professionals to create a supportive environment and offer appropriate analgesia when women attend their intrauterine device (IUD) fitting procedures."
Experiences

Ava, 20
"I've tried most other contraceptives and they all made me put on weight. My implant in the arm made me gain 20kg. The Mirena was my last option. Finding a place wasn't hard because I have had a consistent sexual health clinic that I've been going to since I was 15. They were helpful but it's because I'm very open. As for insertion, that was entirely different.
"I should've been put under general anaesthetic. I screamed for 30 minutes. It was incredibly painful and I have a high pain tolerance because I've had a polypectomy before.
"Afterwards, I was unable to move for three days. It wasn't even my doctor's fault. I don't harbour any ill will because she was trying to help me not be in pain as much as possible, but it was excruciating."
Vicky, 24
"I had the copper coil and it was fine until 18 months in. After that I’d bleed all the time, I was in immense pain after sex. It felt like terrible period cramps all the time."
Yasmin, 28
"I felt embarrassed and awkward, I had a smear test before. I think the reason why I was embarrassed was that I usually keep down there very private and I don’t really talk openly about things unless it’s with parents or my partner.
"They gave me gas and air which really helped to calm me down. The nurse just told me to relax.
"I couldn’t go and do my exercise classes all of that week or have sex until a week later. I took strong painkillers for the rest of the week and codeine for 24hrs after.
"The initial 24hrs after it was done I was in so much pain, but I was told it was normal. The only way I could describe it is that it was like having a constant contraction or stabbing pain."
Charlotte, 23
"I had three attempts of the coil fitted on three different occasions. The first two were unsuccessful due to where I was in my ovulation cycle and I wasn’t made aware that this would be an issue.
"When I had the copper coil fitted they used a local anaesthetic gel which I found useful, however, due to the difficulty during insertion it didn’t last very long.
"The process of insertion is uncomfortable. I felt completely dignified when I had my coil inserted. I had a doctor and a nurse with me who held my hand.
"I do think there should be more post-procedure pain relief offered as over the counter pain medication did not work."
Lexi, 22
"When I went to have the copper coil removed and the kyleena inserted I was told I would find it more painful than initial insertion.
"I was fine but following the insertion, the nurse told me she was surprised I didn't crawl off the table because it's meant to be so severe. I wasn't offered anything for relief."
Alice, 23
"The procedure was fairly painful but it didn’t last long. I remember feeling a bit faint afterwards and they made me lie down for a bit.
"Once I felt ok I went back home, but then the cramp started and I was totally immobilised.
"For the rest of the day and all through the night I was just lying on my bed in the foetal position and weeping.
"I find it hard to remember the pain now because it was five years ago, but I do remember at the time thinking this is the worst pain I’ve ever experienced. I took standard over-the-counter pain killers but they didn’t do much."

The Future of IUDs
As a ministerial foreword in the Women’s Health Strategy The Rt Hon Matt Hancock MP said:
“For generations, women have lived with a health and care system that is mostly designed by men, for men.
“This has meant that not enough is known about conditions that only affect women, or about how conditions that affect both men and women impact women in different ways.
"Pregnant women and women of childbearing age are also under-represented in clinical trials, which can create troubling gaps in data and understanding.
“There’s a lot of great work already underway.
"This government is working on plans for a new Sexual and Reproductive Health Strategy, which we plan to publish later this year.
“We know that not all women have the same experiences, so we want to hear from as many women as possible from all ages and backgrounds about what you think works well and what we need to change.”
Section 5 of the strategy is resolved on ‘Ensuring research, evidence and data supports improvements in women’s health’ and states that: “Women have been under-represented in research, particularly women of ethnic minorities, older women and women of child-bearing age, those with disabilities and LGBT+ women.
"This has implications for the health and care they receive, their options and awareness of treatments, and the support they can access afterwards.”
To try and resolve these issues the health and social care department conducted a survey which ended on the 13th of June. It asked questions including; which women’s health topics do you think the strategy should cover? and how comfortable do you feel talking about health issues with friends and care professionals?
The strategy has not yet been published but Dr Edward Morris, President at the Royal College of Obstetricians and Gynaecologists has called on the government to address this in their new strategy as has Cohen and other pressure groups.
Cohen said: "Governments and devolved nations need to step up and say, right, we hear you, we're going to do something.
"I need people to keep signing the petition and I need people to keep telling their stories. The FSRH are starting to listen but I need the medical profession as a whole to pay this more attention."
Cohen went onto explain that she's been working with Minister of State for Mental Health, Nadine Dorries to provide ideas and research for Women's Health England. She's also working with the fair treatment for women in Wales and patients safety learning groups.
