Understanding Premenstrual Dysphoric Disorder
The silent struggle robbing women of their future

It comes like clockwork. Two weeks of rush. Two weeks of waking up the kids, making breakfast, rushing out to work. Long days in meetings, long evenings with friends. Then the shoe drops. Everything tunes down to a lower frequency. Call into work sick. Tears followed by numbness. Call mum to look after the kids. Pack a suitcase. Think about leaving, not sure where. Retreat to bed. Stay there. Will it pass?

PMS - Premenstrual Syndrome - refers to a spectrum of psychological and physical symptoms that occur during the luteal phase of the menstrual cycle, just after ovulation. According to the American Congress of Obstetricians and Gynecologists, 30% of women – or assigned at birth females – of a reproductive age are affected by premenstrual symptoms. For some people who experience PMS, it can develop into something darker, more forceful, and more destructive: Premenstrual Dysphoric Disorder (PMDD).
Dr Hannah Short, a specialist in menopause and premenstrual disorders, said: “In PMDD, more of the focus tends to be on the emotional symptoms and the behavioural changes that can occur. It's classed mainly as a psychiatric disorder, but it's a bit more complex than that.

Dr. Hannah Short, GP Specialist in Menopause, POI & Premenstrual Disorders Credit: Hannah Short
Dr. Hannah Short, GP Specialist in Menopause, POI & Premenstrual Disorders Credit: Hannah Short
"The symptoms that really trigger the most distress, and why women reach out for help, is a matter of degree.
"Someone with PMS might feel a bit more irritable, maybe a bit tired and low, but if you have PMDD, that could be a real depression, all the irritability could become rage, and the low moods can tip you almost into states of self harm and suicide.
"Anxiety can turn into panic attacks, and women with OCD tendencies can have intrusive thoughts that aren’t there the rest of the time.
"It has such a significant impact on their quality of life and their ability to function, and that’s really how we tend to distinguish the two."
Hormones are chemical messengers that control various bodily functions, including metabolism, growth, reproduction, and mood.
In the ovulation phase, follicle-stimulating hormone (FSH), is secreted, which stimulates follicles in the ovaries that produce eggs.
The hormone estradiol rises, which helps to suppress cortisol, typically causing a boost in happiness and energy.
Ovulation is followed by the luteal phase. Progesterone begins to rise, boosting cortisol production – the body's main stress hormone – which controls mood, motivation and fear.
Sufferers of PMDD have a neurobiological sensitivity to this normal, hormonal transition, which can lead to severe psychiatric symptoms such as paranoia, anxiety, and depresssion. Dr Tory Eisenlour-Moul provides a succint summary of PMDD in the below bitesize overview:

"The brain is having an abnormal reaction to normal hormonal changes. The key thing is that it isn’t a hormonal imbalance."
-Dr. Hannah Short
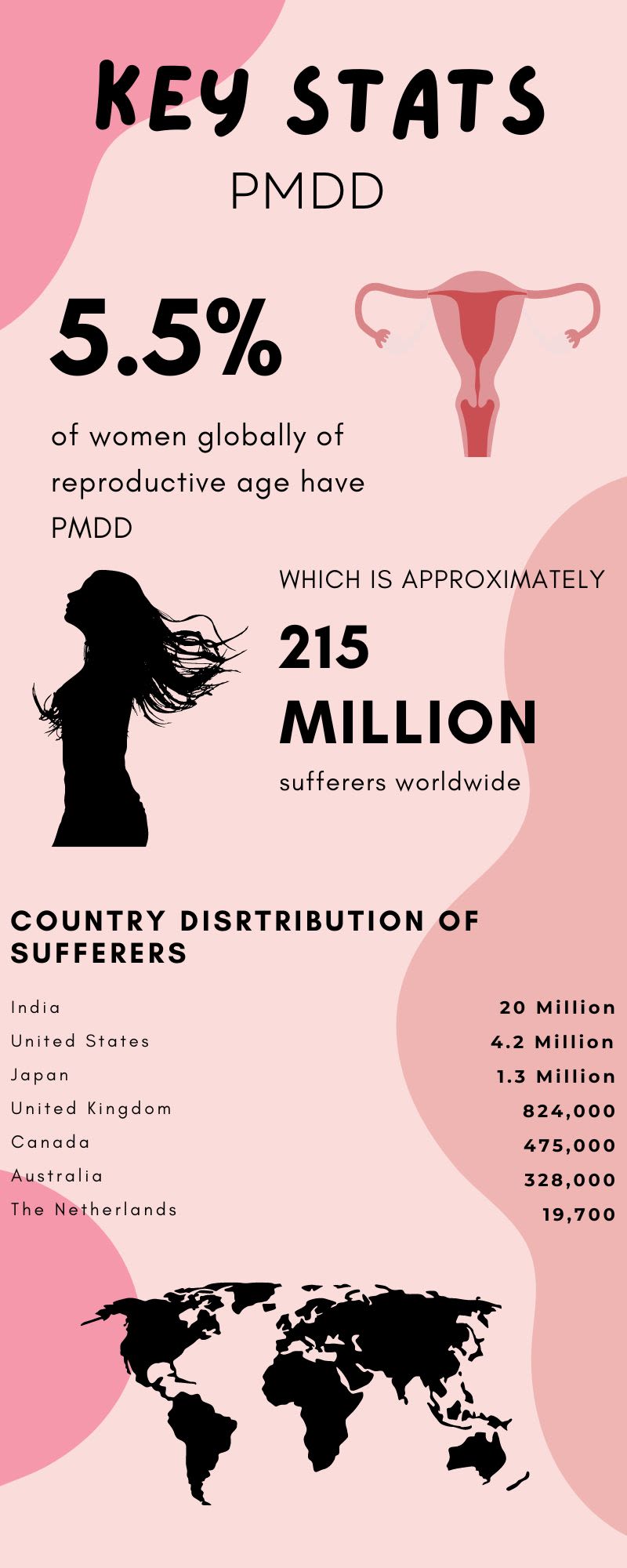
In June 2022, a study published by BMC Psychiatry reported that out of 599 respondents with PMDD, 34% had attempted suicide.
The study was conducted by the International Association for Premenstrual Disorders, Me v PMDD, and Vicious Cycle, and assessed respondents from over 56 countries.
The rates of suicidal ideation and attempt, as shown in the graph above, highlight the extent of debilitating psychiatric symptoms PMDD sufferers endure.
It is quite literally a life-threatening disorder.
The same study also revealed that it takes – on average – 12 years for patients to receive an accurate diagnosis of PMDD.

Symptoms

Psychological Symptoms
Neurological Symptons
Skin Problems
Vascular Symptoms
Urinary Symptoms
Gastrointestinal Symptoms
Breast Symptoms
Uterus Symptoms
Bodily Symptoms
Hannah, depicted in the video above for the BBC, graduated from medical school in her early 30s with a keen interest in psychiatry and mind-body connection. Exposed to the grim state of mental health services at the time, Hannah then went into general practice with the intention of giving her patients a more holistic overview, and consideration of how mental health can impact physical health, and vice versa.
She said: “In medicine, there’s a real tendency to separate mental health from physical health, but you can't really do that. If you’re diagnosed with diabetes, that has an emotional and mental health impact as well. A lot of people with any chronic condition would say that. People with rheumatoid arthritis tend to have a higher rate of depression, and it's not just because they’ve got a chronic condition that’s getting them down, but because there’s a physical process that’s affecting the brain, so it’s a real false dichotomy.”
In psychiatry, Hannah noticed that women’s mental state would fluctuate depending on where they were in their cycle, and this became even more apparent in general practice. She started research to understand how much hormones can impact mind, body, and behaviour – as well as general wellbeing – right across the reproductive lifespan and post-reproductive lifespan.
Her experience as a GP pushed her to branch out into the specialism, and she set up her own private Menopause & Premenstrual Disorders Clinic in Norfolk. Hannah’s comprehensive and holistic approach helps women suffering with severe and complex symptoms of female hormonal health. Hannah’s own journey also contributed to her desire to increase understanding and awareness within the medical profession.
She said: “I had endometriosis and ended up having a hysterectomy when I was 35, and had my ovaries removed. It brought me into stark reality and highlighted how difficult it was even for me, as a medic, to get the help I needed to manage my own symptoms. I found it difficult enough in a relatively privileged position, and realised there’s a lot more work we needed to do.”
Severe symptoms of pre-menstural disorders can be triggered by any traumatic hormonal-related event, which includes puberty, childbirth, miscarriage, abortion, menopause, sterilisation, or starting the contraceptive pill. When a woman’s body goes through a period of hormonal change, the brain can have an abnormal response, which can result in severe psychological distress or behavioural change, symptomatic of PMDD.
Hannah also offers support for women suffering with Premenstrual Exacerbation (PME), which can apply to both physical or mental health conditions. A pre-existing condition can become much worse in the luteal phase of the menstrual cycle. For example, someone suffering with rheumatoid athritis may experience a significant increase in pain during the luteal phase. Equally, someone with a pre-existing psychiatric disorder may suffer worse symptoms in the lead up to their period.
Hannah said: “PME and PMDD often coexist and I think this can be difficult for women trying to get a clear cut diagnosis, because it often takes many years for women to get their diagnosis recognised. Because of the nature of the condition – something that comes round once a month – you're only just getting over it when you get back into another cycle, so you’re going to get concurrent depression and anxiety. It's a natural reaction to develop a mood disorder, especially if you haven't had the help and support from medical professionals."
Hannah’s work endeavours to shine a light on a problem women may have spent years struggling with before receiving a clear diagnosis, and proper support and treatment.
Yet this specialised service is not widely accessible through mainstream health services, due to a lack of funding and awareness.
“I don't remember it being discussed during my training and I think as medical professionals, it would be very good if every time people were admitted to hospital, we could ask where they are in their menstrual cycle or menopause, or are they still having periods, because we’d find with a lot of admissions to A&E – like self-harm – that there could be a relation."


History

The National Association for Premenstrual Syndromes (NAPS) was set up in 1984 to provide information, advice and support to PMS and PMDD sufferers and their families.
NAPS promotes better understanding of both PMS and PMDD, their treatment by the medical profession, and encourages research where appropriate.
Jackie Howe, CEO of NAPS, has worked with the charity since its inception and experienced PMDD and postnatal depression after childbirth.
She said: “I kept a diary and could see that for me, it started at ovulation very severely, with depression. It’s not unusual that it can happen after having a child. I can’t even explain the fatigue - it’s like nothing you could imagine. I also used to get really bad tingling in my body. A lot of women get bloated very badly. It's a horrible condition.”
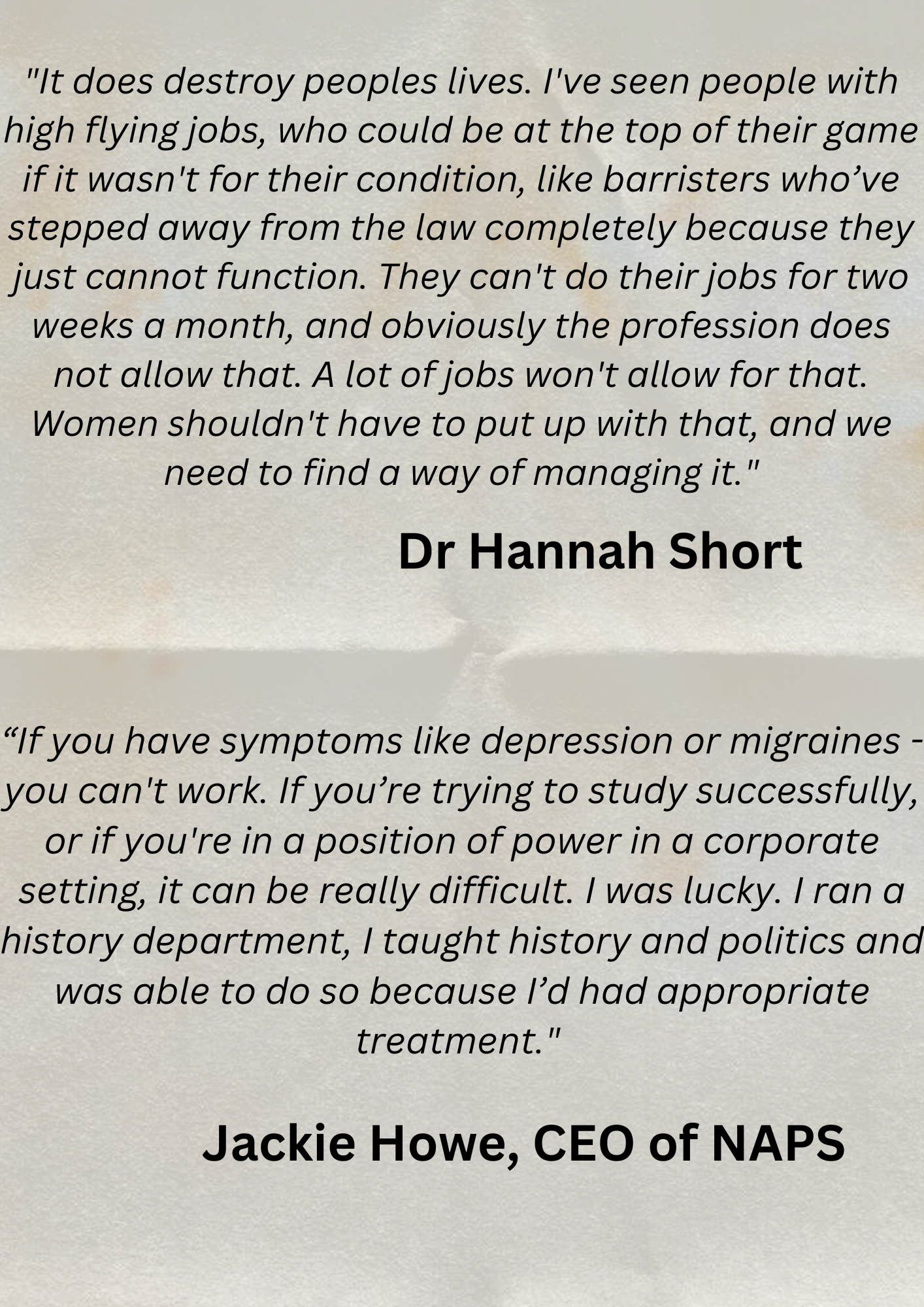
Jackie’s work with NAPS has exposed her to the cruel impact PMDD has on its sufferers.
Despite the pervasive nature of the disorder, many women –such as Ruth – have been able to manage their symptoms with support from NAPS.
The work of NAPS has been integral to increasing awareness of the disorder, and the charity itself was pioneered by the work of Dr Katharina Dalton.
As a GP in North London, Dr Dalton was aware of women presenting with symptoms on a monthly basis and this, combined with experiencing PMS herself, provided the starting point for her to set up a PMS clinic in London.
She also began to run an NHS PMS clinic in University Hospital London, undertake studies on PMS, and champion the cause of women who were desperate to find a treatment for their condition.
In the course of her career, many thousands of PMS sufferers benefitted directly from her treatment as patients, while countless others found help as a result of improved awareness.
Dr Dalton’s book ‘Once a Month’ (first published in 1978) rang immediate bells with sufferers and was sold in huge numbers.
In 1977, Dr Dalton appeared on a TV programme, ‘Pull Yourself Together Woman’, watched by an estimated 11 million viewers, which highlighted the vast numbers of women who were looking for an answer to their severe PMS.
Jackie said: “Katharina Dalton was the woman who made my life possible. I discovered her by chance by reading her book Once a Month.
“She made a huge difference and because of that, we started the charity as a thank you to Katharina Dalton, and to make sure other women didn't suffer like we did, and so that other women could be treated appropriately. It wasn’t just a patient group, it was also set up to work with the medical profession to improve quality care and encourage research.”
As with Hannah, Jackie and the team at NAPS are troubled by the severe lack of awareness of PMDD within mainstream healthcare.
NAPS were asked to contribute to a governmental women’s health strategy: “When the report came out, there was only one line on pre-menstrual syndromes. We couldn’t believe it. To think, there’s an estimated 800,000 women with PMDD in the UK, and there was one line.”
As well as hosting webinars and education days for healthcare professionals, NAPS fund research carried out with their medical trustees. Their website also provides sufferers with advice on approaching their GP, understanding their symptoms, treatment plans, and personal stories from women who have benefitted from NAPS’s support.
Jackie’s work has also connected her with Nikki Owen, who founded The Healing Hub App in 2020 after experiencing the devastating consequences of severe hormonal sensitivity, as detailed on the right.
The app is the result of three decades of tools and techniques pioneered by Owen, who claims to have successfully treated thousands of individuals combining breath-work, sound therapy, neuro-linguistic programming and hypnosis.
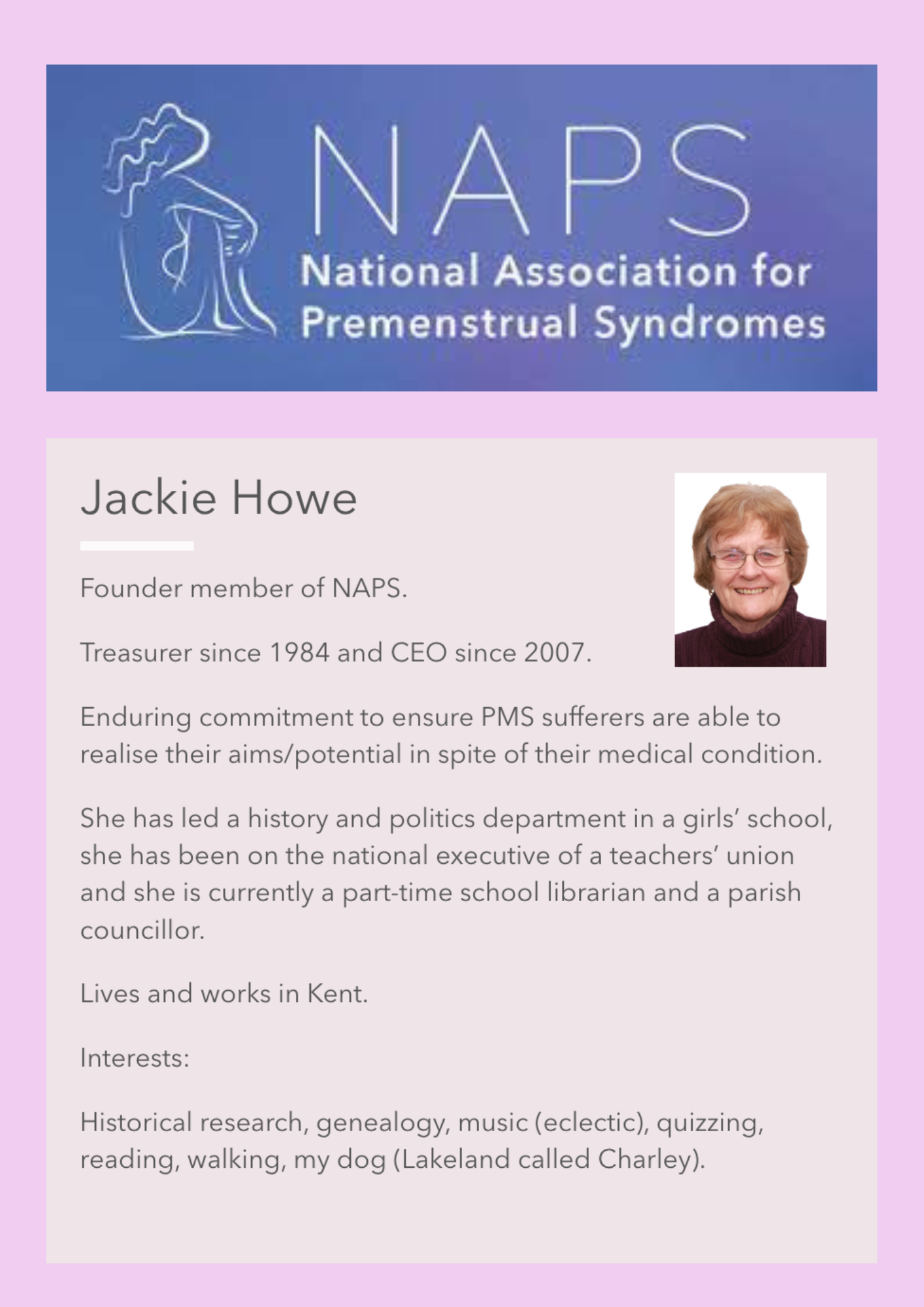
Image credit: NAPS
Image credit: NAPS
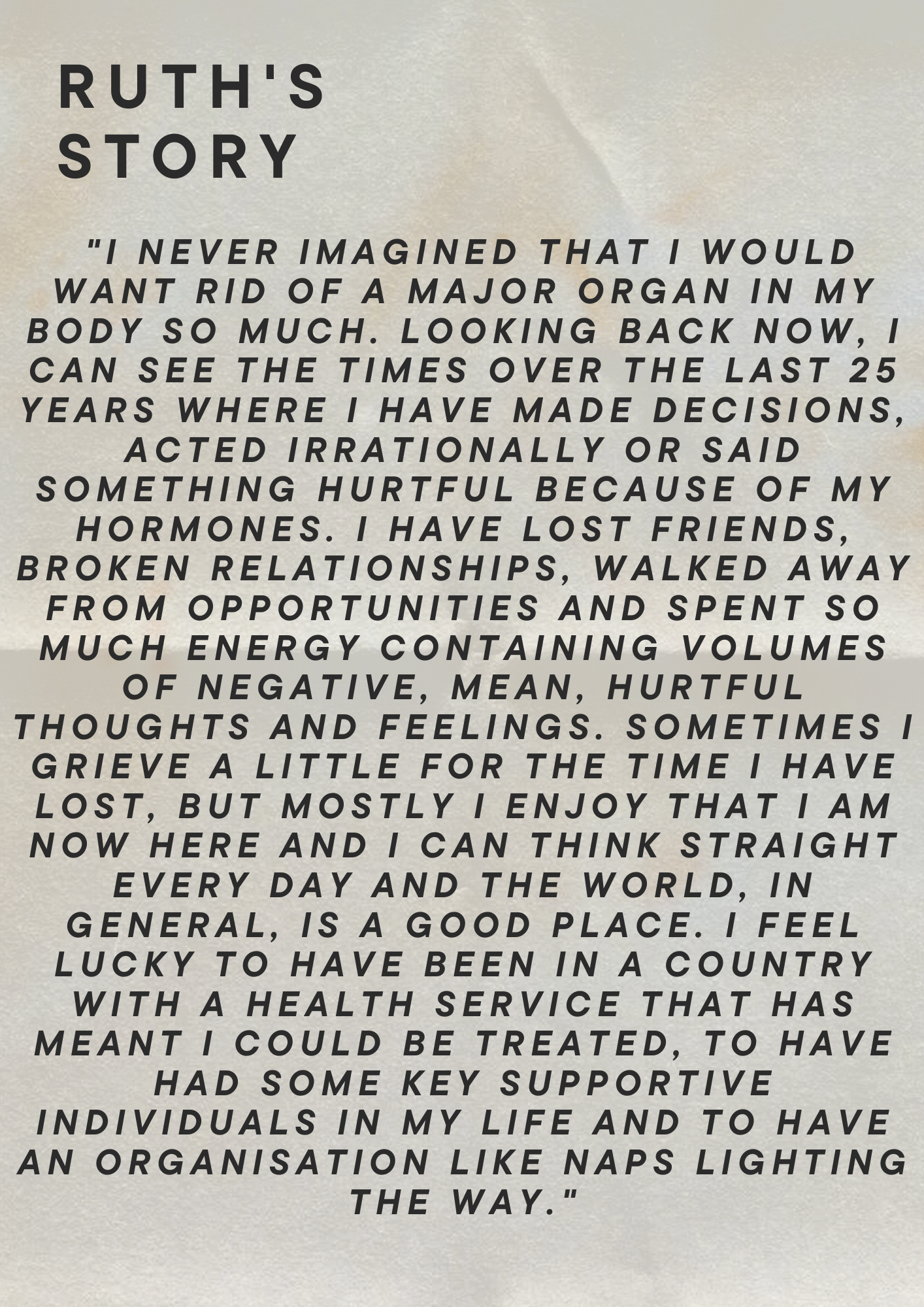
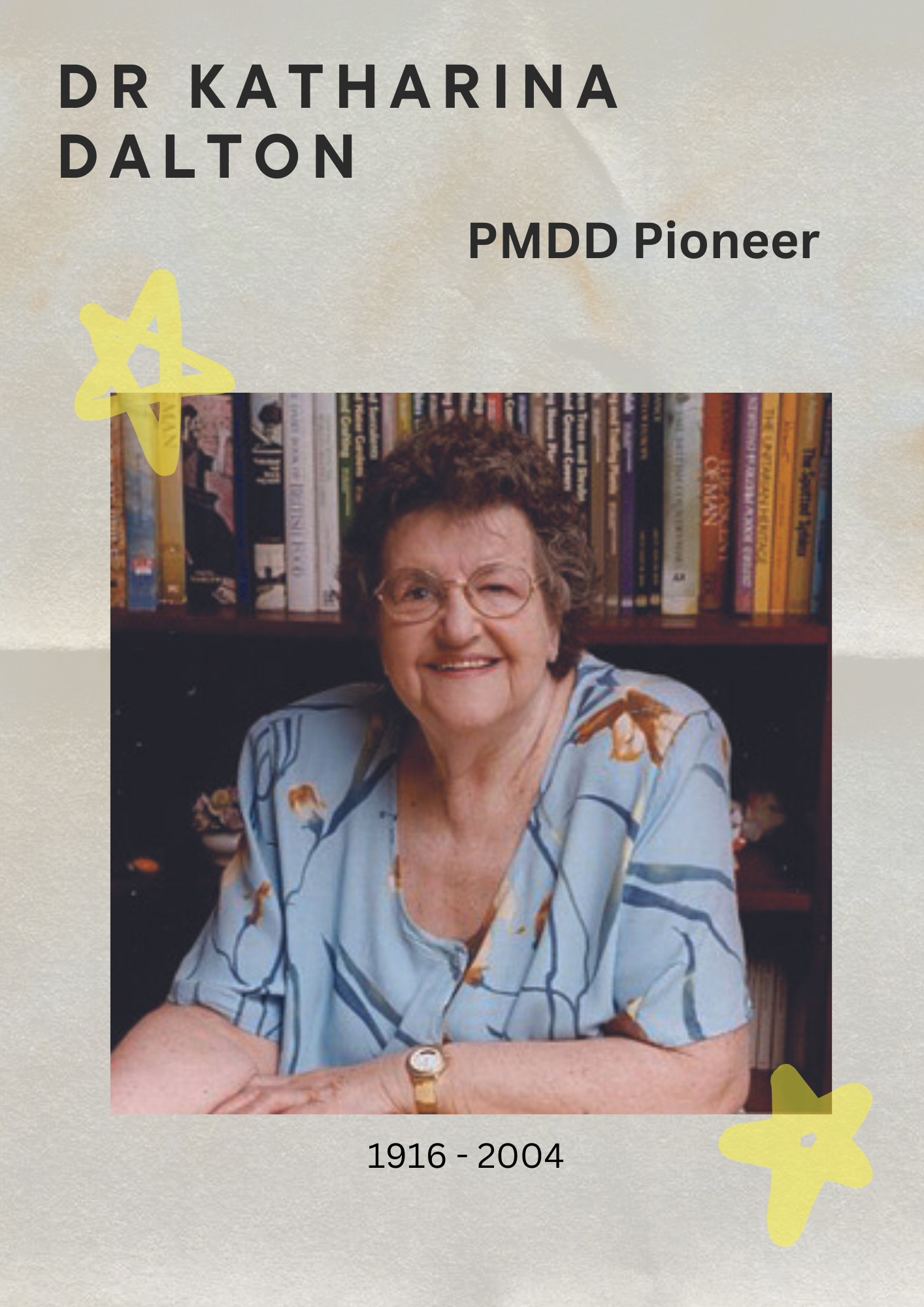
Image credit: NAPS
Image credit: NAPS
PMDD & Neurodiversity

Samantha Hiew, Keynote Speaker and Founder of ADHD Girls Credit: Samantha Hiew
Samantha Hiew, Keynote Speaker and Founder of ADHD Girls Credit: Samantha Hiew
She founded ADHD Girls before she herself was diagnosed with attention deficit hyperactivity disorder, and started interviewing women across the world to find out about their stories.
Her campaign snowballed into the formation of ADHD Girls – an online community which offers education and empowerment. It’s a space where neurodivergent women can ask each other questions about medications, diet, lifestyle and navigating professional and personal relationships.
Samantha also gives talks and training about neurodiversity in the workplace.
“There was a lot of learning along the way which I share in my community, and now I give a lot of talks on ADHD and women. These sessions are always very impactful and powerful, because it's just nice to be in a room where people feel this sense of community. Most of us find it a bit of a mission to go out and meet other people, so it's nice that when you do, you feel validated in this space.”
From gathering anecdotes from women across the globe, Samantha soon noticed the relationship between neurodiversity and hormonal sensitivity. Her research suggested a link between neurobiological sensitivity present in PMDD and neurodivergent women.
The first study conducted to acknowledge this connection was published in 2021, in the Journal of Psychiatric Research (Volume 133).

Samantha Hiew discusses the effect of PMDD & Neurodiversity on cognitive function
Samantha Hiew discusses the effect of PMDD & Neurodiversity on cognitive function
PMDD in the Workplace
The impact of PMDD on cognitive and emotional function can have serious implications for women’s careers, and was raised by both Hannah Short and Jackie Howe.
Already campaigning for greater support for neurodivergency in the workplace, Samantha Hiew's mission has extended to increasing awareness of the impact of hormonal sensitivity on intellectual productivity.
Samantha Hiew discusses what can be done to support women in the workplace suffering with hormonal sensitvity.
Samantha Hiew discusses what can be done to support women in the workplace suffering with hormonal sensitvity.
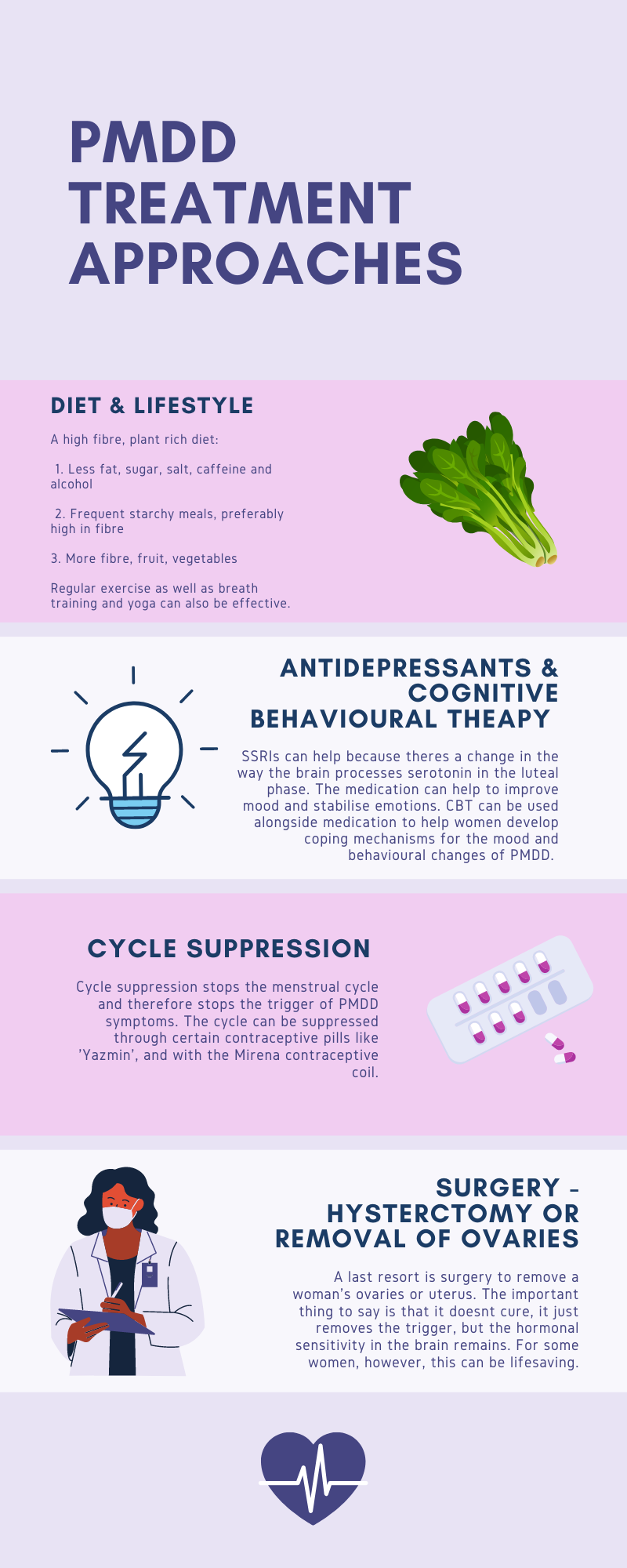
Treatment

Treatment of PMDD is tailored to individual sufferers, and different approaches can be taken depending on the degree and prevalence of psychiatric symptoms.
The process starts with ruling out anything that could be causing a hormonal imbalance, such as thyroid issues or polycystic ovaries.
Although the menstrual cycle is the trigger of PMDD, it’s not the cause of the condition. Treatment often begins with looking at a dietary and lifestyle approach.
The strands of symptom management are changing or altering the brain's reaction to the hormonal changes which trigger the symptoms.
Women with PMDD can have a higher level of chronic inflammation at the cellular level, so dietary recommendations like a high fibre plant rich diet can be effective due to the impact on gut health, blood sugar regulation, and the way the body deals with the breakdown products of hormones.
But a naturopathic approach is not always a cure-all, as Hannah Short explains:


Final Thoughts
Recognition of PMDD in mainstream healthcare and psychiatry has only occured in the last decade. PMDD was added to the American Psychiatric Association's Diagnostic Manual in 2013, after several studies showed PMDD was caused by a brain hormone sensitivity, rather than hormonal imbalance.
Later in 2019, the World Health Organisation then added PMDD to its international classification of diseases. Yet the work of Katharina Dalton in the 1970s proves that – to its sufferers – PMDD is not a novel illness. Patients are often aggrieved with a long and painful process to reach a clear diagnosis.
Women's hormonal health continues to be an underfunded and overlooked area of mainstream medicine, which is why the work of doctors like Hannah is so vital. Not all patients, however, have the financial means to access adequate and specialised treatment.
The statistic that 34% of sufferers had attempted suicide speaks volumes about the work that remains to be done. Hannah confessed her hope that one day, women will no longer have to resort to hysterectomies to alleviate them of the intense distress of PMDD. For some women, however, it is their last chance of survival.
The work of NAPS and noisemakers like Samantha does show that there is room for hope. More awareness carries the promise of greater understanding and subsequent changes to policy and funding.
If you believe you may be suffering with PMDD, there is help out there, and you aren't alone.
Words of Wisdom

The contributors to this story have each shared their advice to women suffering with premenstrual symptoms.

Dr Hannah Short
"If anybody thinks it could relate to them, the key thing to do is to start tracking symptoms. There should be quite a clear pattern if it is PMDD. The difficulty comes if you have irregular periods, but then that's very key to track because you can notice if you do have a period where you're feeling bad just before that, and each time that will be telling. Normally track two cycles minimum and go to your GP. Look for resources on IAMPD and NAPS. It is getting more awarness in the medical profession, but it can be overwhelming."

Jackie Howe
"My advice would be for women to take a friend or partner with them when they first approach a doctor. Sometimes if it's a male doctor, or someone who doesn't have a strong understanding of PMDD or hormonal sensitivities, you can be quite quickly dismissed, and we’ve spoken to many women who had this experience, and have felt browbeaten. I spoke to a GP once who said ‘the problem with PMS is that it takes so long to deal with’, and I said, ‘Try being the patient.’ The dietary approach is important. You should go for complex carbohydrates, and not wait too long between meals. It’s important to think about blood sugar, and eat regularly."

Dr Samantha Hiew
"I would look at what the stress points are in your life, as we know that stress impacts your sex hormones which then impacts your dopamine, so what we should do is to get curious, and to try and find out as much as you can about this and track your cycle. If your challenges come at certain parts of the month you should understand why that's happening, and the first thing to do is get a menstrual tracker app. Some people I know have turned to naturopathic strategies – no studies have been truly done, but they say it's helped. So there are various ways people have found to help them, but I think having a balanced nutrition that coincides with different parts of your cycle will really help."


